Avascular Necrosis
Avascular necrosis (AVN), also called osteonecrosis, is a condition in which bone tissue dies due to an insufficient blood supply. This lack of blood flow causes the bone to weaken, collapse, and lose its smooth structure. The hip joint, specifically the femoral head, is one of the most common sites affected by AVN. If untreated, the condition can lead to severe arthritis and loss of joint function.
How Common It Is and Who Gets It? (Epidemiology)
Avascular necrosis can affect anyone but is most common in adults between the ages of 30 and 50. It is seen more frequently in patients with a history of hip trauma, steroid use, or heavy alcohol consumption. Men are affected slightly more often than women. The hip is the most frequently involved site, but AVN can also affect the shoulder, knee, or ankle.
Why It Happens – Causes (Etiology and Pathophysiology)
AVN occurs when the blood supply to the bone is disrupted or reduced. Without sufficient oxygen and nutrients, bone cells die, and the bone structure begins to collapse. Common causes include:
-
Trauma: Fractures or dislocations of the hip can damage nearby blood vessels.
-
Medications: Long-term use of corticosteroids like prednisone increases lipid levels in the blood, which can block blood vessels.
-
Alcohol: Heavy, prolonged drinking may cause fat deposits to build up in blood vessels, reducing circulation to the bone.
-
Radiation or chemotherapy: Cancer treatments can weaken bone and harm the vascular supply.
-
Medical conditions: Sickle cell anemia, lupus, Gaucher disease, antiphospholipid syndrome, and pancreatitis can interfere with bone blood flow.
In some cases, the cause is unknown, known as idiopathic AVN.
How the Body Part Normally Works? (Relevant Anatomy)
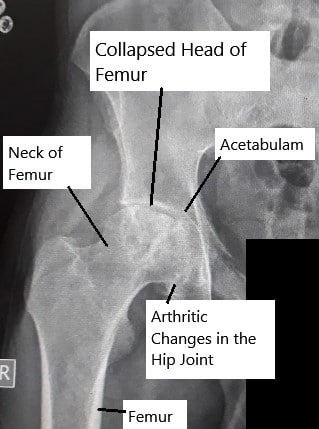
The hip joint is a ball-and-socket joint formed by the femoral head (ball) and the acetabulum (socket). The femoral head receives its blood supply through small arteries that run along the neck of the femur. When these arteries are disrupted or compressed, the blood flow stops, leading to bone death in the femoral head. Over time, the joint loses its round shape, causing pain and stiffness.
What You Might Feel – Symptoms (Clinical Presentation)
Early stages of AVN may cause mild or no symptoms. As the condition progresses, pain becomes more noticeable:
-
Hip pain is the most common symptom, often felt in the groin, thigh, or buttock.
-
Pain initially occurs during weight-bearing but can later occur even at rest or while lying down.
-
Limited motion or stiffness develops as the bone and joint deteriorate.
-
In advanced stages, limping and difficulty walking are common.
AVN can affect one or both hips simultaneously.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis starts with a detailed medical history and physical examination. Your doctor may suspect AVN based on your risk factors and symptoms.
-
X-rays may appear normal in the early stages but later show bone collapse and irregular joint surfaces.
-
MRI scans are the most sensitive imaging tests, detecting early changes before they appear on X-rays.
-
CT scans show bone detail and help evaluate the extent of bone damage.
-
Bone scans can also confirm decreased bone activity in the affected region.
Classification
AVN is typically classified by the stage of disease progression:
-
Stage I: Normal X-ray, but MRI shows early bone changes.
-
Stage II: X-ray shows sclerosis (hardening) or cysts, but the bone contour is intact.
-
Stage III: Subchondral fracture (“crescent sign”) indicates bone collapse under the cartilage.
-
Stage IV: Advanced collapse of the femoral head and arthritis of the hip joint.
These stages help guide treatment decisions.
Other Problems That Can Feel Similar (Differential Diagnosis)
AVN can mimic other causes of hip pain such as transient osteoporosis, hip arthritis, labral tears, or stress fractures. Imaging is key to differentiating these conditions.
Treatment Options
Non-Surgical Care – Early-stage AVN may be managed conservatively:
-
Limiting weight-bearing with crutches or a cane to reduce stress on the hip.
-
Medications such as NSAIDs to relieve pain.
-
Treatment of underlying causes (e.g., adjusting steroid or alcohol use).
-
Physical therapy to maintain motion and muscle strength.
-
Bisphosphonate therapy in select patients to prevent bone collapse.
Surgical Care – Surgery is often required for advanced stages:
-
Core decompression: A small hole is drilled into the bone to relieve pressure and stimulate new blood vessel growth.
-
Bone grafting: Healthy bone is transplanted to replace damaged tissue.
-
Osteotomy: Bone is repositioned to shift weight away from the damaged area.
-
Hip replacement (arthroplasty): In advanced cases, replacing the damaged femoral head and acetabulum restores movement and eliminates pain.
-
Fusion (arthrodesis): Rarely used for severe, non-reconstructable cases.
Recovery and What to Expect After Treatment
Recovery depends on the stage and treatment method. Early-detected AVN treated non-surgically may take several months to resolve. After surgery, physical therapy is crucial to restore range of motion and strength. Patients undergoing hip replacement typically resume daily activities within a few months, with pain relief beginning soon after surgery.
Possible Risks or Side Effects (Complications)
Untreated AVN can progress to bone collapse and severe arthritis. Surgical risks include infection, implant loosening, and nerve or vessel injury. In advanced cases, the bone deformity can cause permanent loss of hip mobility.
Long-Term Outlook (Prognosis)
The prognosis depends on early detection and the severity of the disease. When diagnosed early, non-surgical treatments can preserve the joint and prevent collapse. In later stages, total hip replacement offers excellent long-term outcomes for pain relief and mobility restoration.
Out-of-Pocket Costs
Medicare
CPT Code 20902 – Bone Grafting (Harvest and Placement of Bone Graft): $63.66
CPT Codes 27125 / 27130 – Hip Replacement (Partial / Total Hip Arthroplasty): $268.14 / $303.45
CPT Code 38220 – Bone Marrow Injection (Aspiration for Bone Marrow Concentrate Therapy): $36.05
Medicare Part B typically covers 80% of the approved cost for these procedures once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries and procedures. These plans coordinate with Medicare to close the coverage gap and reduce patient financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans usually cover any remaining coinsurance or small deductibles, which typically range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your avascular necrosis developed as a result of a work-related injury, steroid exposure, or trauma, Workers’ Compensation will cover all associated medical expenses, including surgery, bone grafting, and rehabilitation. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip condition or bone damage related to avascular necrosis resulted from an automobile accident, No-Fault Insurance will typically cover the full cost of your treatment, including joint replacement, bone grafting, or marrow injections. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
David Chen was diagnosed with avascular necrosis of the femoral head and underwent core decompression with bone grafting (CPT 20902), followed by a total hip replacement (CPT 27130) due to joint collapse. His estimated Medicare out-of-pocket costs were $63.66 for the bone graft and $303.45 for the total hip arthroplasty. Since David had supplemental insurance through Blue Cross Blue Shield, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for either procedure.
Frequently Asked Questions (FAQ)
Q. Can avascular necrosis heal on its own?
A. In very early stages, reducing weight-bearing and addressing the underlying cause may allow partial healing, but advanced stages often require surgery.
Q. Is avascular necrosis the same as arthritis?
A. No. AVN causes bone death, which can later lead to arthritis, but the initial process involves loss of blood supply, not joint inflammation.
Q. Can both hips be affected?
A. Yes, AVN often affects both hips, sometimes at different stages of progression.
Summary and Takeaway
Avascular necrosis is a serious condition in which the bone loses its blood supply, leading to bone death and eventual joint collapse. Early diagnosis and treatment are critical to preserving bone health. Advanced cases may require surgical intervention such as hip replacement to restore function and relieve pain.
Clinical Insight & Recent Findings
Avascular necrosis (AVN) is a serious condition that affects the femoral head, leading to the potential need for total hip arthroplasty (THA). While THA is a common and effective treatment, it may not be ideal for younger, more active patients due to the risk of needing revision surgeries later in life.
A recent systematic review highlighted the role of orthobiologic therapies, such as bone marrow aspirate concentrate (BMAC), in delaying the need for hip replacement surgery. The study found that BMAC, in particular, significantly improved long-term survival without the need for THA, providing a promising alternative for managing AVN.
These findings suggest that early intervention with orthobiologics could help preserve the natural hip joint and delay more invasive procedures like THA. (“Study on orthobiologic therapies delaying hip replacement surgery in AVN – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Avascular necrosis is managed by orthopedic surgeons specializing in hip disorders. Radiologists assist in diagnosis, and physical therapists play a vital role in postoperative rehabilitation. Primary care physicians and rheumatologists may be involved in managing underlying risk factors.
When to See a Specialist?
If you experience persistent hip or groin pain that worsens with activity, or if pain continues despite rest, consult an orthopedic specialist. Early evaluation can prevent further bone damage.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience sudden hip pain after trauma or dislocation, as this may indicate a loss of blood flow to the bone.
What Recovery Really Looks Like?
Recovery varies depending on disease stage and treatment type. Patients undergoing early-stage interventions may return to activity within months, while those with hip replacement typically achieve full recovery in 3–6 months with physical therapy.
What Happens If You Ignore It?
Ignoring avascular necrosis can result in progressive bone collapse, chronic pain, and permanent joint deformity. Left untreated, it nearly always leads to disabling arthritis requiring joint replacement.
How to Prevent It?
To reduce the risk of AVN:
-
Avoid excessive alcohol consumption.
-
Monitor and limit steroid use under medical supervision.
-
Maintain healthy cholesterol levels to prevent fat blockages.
-
Avoid smoking, which constricts blood vessels and reduces bone perfusion.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and protein supports bone healing and density. Staying hydrated and maintaining a balanced diet with limited alcohol and caffeine further helps bone circulation.
Activity and Lifestyle Modifications
Low-impact exercises like swimming or cycling help maintain joint mobility. Avoid high-impact activities that stress the hip joint. Following your doctor’s advice on weight-bearing limits and physical therapy enhances long-term hip health.

Dr. Sebastian Heaven
I provide Orthopaedic patient care at several different locations, including a Regional Joint Assessment Centre, a Level 1 Trauma Centre and a District General Hospital. My scope of practice is broad and includes Trauma, Arthroplasty and Sports Orthopaedics.
My areas of special interest include Primary and Revision Arthroplasty, Periprosthetic Fracture Management and general orthopaedic trauma management in isolation and in the context of complex polytrauma patients. I also have clinical research interests in these areas, as well the development of interprofessional relationships between trauma team members and fellow healthcare professionals.
I have personally written all or most of what's on this page for Complete Orthopedics, and approve the use of my content.
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]