Stem Cell Therapy for Avascular Necrosis of the Hip
Stem cell therapy, a form of regenerative medicine, has gained attention for its potential to treat avascular necrosis (AVN) of the hip. AVN occurs when the blood supply to the head of the femur is disrupted, leading to bone death and collapse of the joint. Stem cells, harvested from the bone marrow, fat, or blood, are injected into the affected area to stimulate bone regeneration, improve blood supply, and delay the need for joint replacement.
How Common It Is and Who Gets It? (Epidemiology)
Avascular necrosis of the hip most commonly affects individuals between the ages of 30 and 50, especially those who are physically active. It is frequently caused by trauma (fractures or dislocations), excessive corticosteroid use, or chronic alcohol abuse. In some cases, medical conditions that affect clotting or blood flow, such as lupus or sickle cell anemia, can also lead to AVN.
Why It Happens – Causes (Etiology and Pathophysiology)
The primary cause of AVN is the disruption of blood flow to the femoral head, either from trauma or non-traumatic causes. As the blood supply is reduced, bone cells die and the bone structure weakens. Over time, this leads to the collapse of the femoral head, resulting in pain, reduced mobility, and arthritis. In the early stages, bone marrow attempts to regenerate new bone, but inadequate blood flow impedes this process.
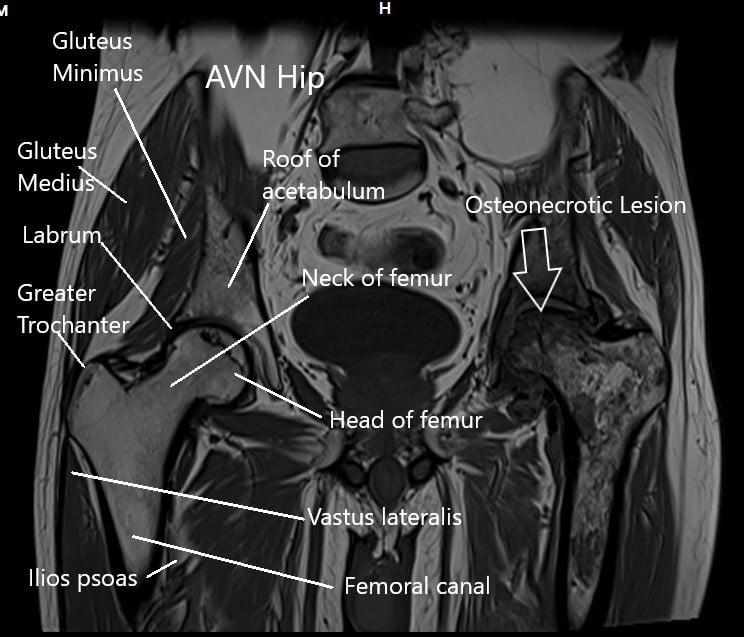
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint, where the femoral head (ball) fits into the acetabulum (socket) of the pelvis. Healthy bone is maintained through a continuous process of bone turnover, supported by a steady blood supply. The femoral head relies on vascularization to receive nutrients and maintain its structure. Without adequate blood flow, the femoral head becomes susceptible to necrosis and collapse.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with AVN of the hip typically experience:
-
Pain: Usually located in the groin or outer thigh, which worsens with movement or weight-bearing activities.
-
Stiffness: Difficulty in moving the hip joint, particularly in activities like walking, squatting, or bending.
-
Limited mobility: The inability to fully rotate or lift the leg, which significantly impacts daily activities.
-
Pain at rest: In more advanced stages, pain may be constant, even during rest.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
Physical examination: A doctor may check for tenderness, restricted movement, and muscle weakness in the hip area.
-
X-rays: Often used to rule out other conditions, though early-stage AVN may not show clear changes.
-
MRI or bone scan: These imaging techniques are more effective in detecting early-stage AVN, where bone changes and damage may not be visible on X-rays.
Procedure Types or Techniques (Classification)
Stem cell therapy for AVN can be used in combination with other joint-preserving treatments, such as:
-
Core decompression: Involves creating small tunnels in the femoral head to relieve pressure and stimulate blood flow.
-
Bone grafting: Bone grafts can be used to help fill the void left by the dead bone and promote healing.
-
Stem cell injection: Bone marrow-derived stem cells are injected into the necrotic area to stimulate regeneration and revascularization.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Osteoarthritis: Causing similar pain and stiffness, but usually seen in older patients and affects the entire joint.
-
Labral tear: Often causes groin pain, but this is typically related to a tear in the cartilage rather than bone damage.
-
Trochanteric bursitis: Inflammation in the hip bursa causing outer hip pain, which can mimic AVN.
Treatment Options
Non-surgical treatments: Physical therapy, pain management (NSAIDs, corticosteroid injections), and activity modification are often used in early-stage AVN.
Surgical options: When symptoms persist, core decompression and stem cell therapy are considered, with hip replacement surgery reserved for more advanced stages.
Recovery and What to Expect After Surgery
-
Postoperative care: Patients are typically advised to limit weight-bearing for 4-6 weeks to allow the bone to heal and the stem cells to work.
-
Physical therapy: Begins shortly after the procedure, focusing on improving hip mobility and strength.
-
Pain management: Post-surgical pain usually subsides within a few weeks, with most patients resuming daily activities after 3-6 months.
-
Follow-up: Regular monitoring through X-rays and MRIs to assess the healing process.
Possible Risks or Side Effects (Complications)
-
Infection: As with any surgical procedure, there is a risk of infection at the injection or surgical site.
-
Graft failure: If bone grafts or stem cells do not integrate properly, the necrosis may progress, requiring additional intervention.
-
Bone collapse: In some cases, AVN may progress despite stem cell therapy, requiring total hip replacement.
Long-Term Outlook (Prognosis)
Stem cell therapy can significantly slow or halt the progression of AVN in the early stages. While many patients experience pain relief and restored function, the long-term success depends on the severity of the AVN and the extent of bone collapse. In some cases, the disease may progress to the point where joint replacement is necessary.
Out-of-Pocket Costs
Medicare
CPT Code 38220 – Bone Marrow Aspiration (Stem Cell Harvest): $36.05
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved procedures. These plans coordinate with Medicare to fill the coverage gap and reduce the patient’s financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it serves as a secondary payer. These plans typically cover any remaining balance, including coinsurance or small deductibles, which generally range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your bone marrow aspiration or stem cell harvest is related to a work injury, Workers’ Compensation will cover all associated medical expenses, including the procedure and any follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your bone marrow aspiration is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Amy Stevens required bone marrow aspiration (CPT 38220) for stem cell therapy as part of a treatment plan for osteoarthritis. Her estimated Medicare out-of-pocket cost was $36.05. Since Amy had supplemental insurance through AARP Medigap, her remaining balance was fully covered, leaving her with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. How long will stem cell therapy last?
A. Stem cell therapy can offer relief for several years, though some patients may eventually require hip replacement.
Q. Is it effective in all patients?
A. Stem cell therapy is most effective in the early stages of AVN and may not be suitable for advanced cases.
Q. Can I return to sports after treatment?
A. Most patients can return to low-impact activities such as swimming or walking, but high-impact activities should be avoided.
Summary and Takeaway
Stem cell therapy offers a promising treatment option for early-stage avascular necrosis, providing pain relief, promoting bone regeneration, and delaying the need for hip replacement. With appropriate patient selection, this approach can significantly improve quality of life and preserve hip function.
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in hip and joint preservation perform stem cell therapy procedures, often in collaboration with physical therapists and anesthesiologists.
When to See a Specialist?
Consult an orthopedic specialist if you experience persistent hip pain, especially if you have risk factors like corticosteroid use or alcohol consumption.
When to Go to the Emergency Room?
Seek medical attention if you experience sudden, severe hip pain, or if you notice signs of infection (fever, redness, swelling) after the procedure.
What Recovery Really Looks Like?
Recovery typically involves gradual weight-bearing, physical therapy, and periodic imaging to monitor progress. Most patients see significant improvement in 3-6 months.
What Happens If You Delay Surgery?
Delaying stem cell therapy or core decompression may lead to joint collapse and the need for more invasive procedures like hip replacement.
How to Prevent Recurrence or Failure?
Maintain a healthy weight, avoid high-impact activities, and continue physical therapy to ensure the best possible outcome.
Nutrition and Bone or Joint Health
A balanced diet rich in calcium and vitamin D helps support bone health. Avoiding smoking and excessive alcohol consumption can also improve outcomes.
Activity and Lifestyle Modifications
Post-treatment, engage in low-impact activities like swimming or cycling to maintain joint health, and avoid heavy lifting or running to protect the hip.
Read more about Avascular Necrosis of the Hip Joint here.
Do you have more questions?
How effective is stem cell therapy compared to other treatments for avascular necrosis of the hip, such as core decompression or joint replacement surgery?
Stem cell therapy is a relatively newer approach for treating avascular necrosis of the hip, and its effectiveness compared to traditional treatments like core decompression or joint replacement surgery is still being evaluated. While some studies and clinical trials have shown promising results in terms of pain relief and improvement in hip function, more research is needed to determine the long-term outcomes and effectiveness of stem cell therapy.
Additionally, the success of any treatment depends on various factors such as the stage of the disease, the patient’s overall health, and the expertise of the healthcare provider performing the procedure. It’s essential to discuss the potential benefits and risks of each treatment option with your orthopedic surgeon to determine the most appropriate course of action for your specific condition.
Are there any risks or complications associated with stem cell therapy for avascular necrosis of the hip?
How long does it typically take to see results from stem cell therapy for avascular necrosis of the hip?
The timeline for seeing results from stem cell therapy for avascular necrosis of the hip can vary depending on several factors, including the severity of the condition, the individual patient’s response to treatment, and whether the therapy is combined with other interventions such as core decompression. In some cases, patients may begin to experience improvements in symptoms within a few weeks to months after the procedure, as the injected stem cells work to repair damaged bone tissue and promote new blood vessel growth.
However, it’s essential to note that stem cell therapy is not a quick fix, and full regeneration of the affected bone may take several months to a year or longer. Regular follow-up appointments with your healthcare provider can help track progress and adjust treatment plans as needed.
Are there any risks or potential complications associated with stem cell therapy for avascular necrosis of the hip?
As with any medical procedure, there are potential risks and complications associated with stem cell therapy for avascular necrosis of the hip. These may include infection at the injection site, allergic reactions to anesthesia or other medications used during the procedure, and the possibility of inadequate or incomplete healing of the affected bone tissue.
Additionally, there may be a risk of unintended effects on surrounding tissues or organs, although such occurrences are rare when the procedure is performed by experienced medical professionals using proper techniques and precautions. It’s essential for patients to discuss these potential risks with their healthcare provider before undergoing treatment and to follow all pre- and post-procedure instructions carefully to minimize the likelihood of complications
Are there any age restrictions or limitations for undergoing stem cell therapy for avascular necrosis of the hip?
Stem cell therapy for avascular necrosis of the hip is generally considered safe and effective across a wide range of age groups. However, the suitability of the treatment may vary based on individual factors such as overall health, bone density, and the extent of hip joint damage. It’s essential for patients to undergo a comprehensive evaluation by a healthcare provider specializing in orthopedics to determine if they are suitable candidates for stem cell therapy.
How long does it typically take to see results after undergoing stem cell therapy for avascular necrosis of the hip?
In most cases, patients may start to notice improvements in their symptoms within a few weeks to months after undergoing stem cell therapy for avascular necrosis of the hip. However, the exact timeline for experiencing significant relief can vary depending on factors such as the extent of bone damage, individual healing response, and adherence to post-procedure rehabilitation protocols. It’s essential for patients to maintain regular follow-up appointments with their healthcare provider to monitor progress and adjust treatment as needed.
Are there any contraindications or medical conditions that would make a patient ineligible for stem cell therapy for avascular necrosis?
Patients with active infections, certain blood disorders, or a history of cancer may be ineligible for stem cell therapy due to increased risks or potential interference with treatment outcomes. Each patient’s medical history is carefully evaluated to determine candidacy.
What measures are taken to ensure the safety and sterility of the stem cell harvesting and injection process?
Strict protocols are followed to maintain sterility during stem cell harvesting and injection procedures. This includes using a sterile environment, proper disinfection of equipment, and adherence to aseptic techniques to minimize the risk of infection.
Can stem cell therapy be performed on both hips simultaneously, or is it typically done one hip at a time?
Stem cell therapy can be performed on both hips simultaneously if both are affected by avascular necrosis. However, the decision to treat one or both hips at the same time depends on factors such as the patient’s overall health and the extent of the disease.
Are there different types of stem cells used in therapy for avascular necrosis, and if so, how do they differ in terms of effectiveness and safety?
The most commonly used stem cells for avascular necrosis are bone marrow-derived mesenchymal stem cells. These have shown effectiveness in promoting bone regeneration and have a favorable safety profile compared to other types of stem cells.
Is stem cell therapy covered by insurance for the treatment of avascular necrosis, or is it considered an elective procedure?
Coverage for stem cell therapy varies depending on the patient’s insurance plan and the specific circumstances of their condition. While some insurance providers may cover it for certain indications, others may consider it elective and not covered.
What is the typical recovery timeline following stem cell therapy for avascular necrosis, and when can patients expect to see improvements in symptoms?
Patients may experience gradual improvements in symptoms over several weeks to months following stem cell therapy. However, individual recovery timelines can vary based on factors such as the extent of bone damage and the patient’s overall health.
Are there any lifestyle modifications or dietary recommendations that can enhance the effectiveness of stem cell therapy for avascular necrosis?
Maintaining a healthy lifestyle with regular exercise and a balanced diet rich in nutrients essential for bone health can support the effectiveness of stem cell therapy. Avoiding smoking and excessive alcohol consumption is also advisable.
How soon after diagnosis should stem cell therapy be initiated for avascular necrosis, and is there an optimal window of opportunity for treatment?
Early intervention with stem cell therapy is preferred, ideally in the early stages of avascular necrosis before significant bone collapse occurs. However, it can still be beneficial in later stages to slow disease progression and alleviate symptoms.
What criteria are used to determine if a patient is a suitable candidate for stem cell therapy for avascular necrosis?
Patient selection criteria typically include factors such as the stage of avascular necrosis, overall health status, response to conservative treatments, and absence of contraindications like active infection or cancer.
Can stem cell therapy be used in combination with other treatments, such as medication or physical therapy, for avascular necrosis of the hip?
Yes, stem cell therapy can be complemented by other treatments like medication for pain management and physical therapy for rehabilitation. Combining therapies may enhance overall outcomes and promote better functional recovery.
Is stem cell therapy considered a permanent solution for avascular necrosis, or are repeat treatments often necessary?
Stem cell therapy can provide long-term relief and potentially halt the progression of avascular necrosis. However, repeat treatments may be necessary for some patients, especially if the condition progresses or if symptoms recur over time.
What are the potential risks or complications associated with stem cell therapy for avascular necrosis?
While stem cell therapy is generally considered safe, potential risks include infection, bleeding, and allergic reactions. Additionally, there is a theoretical risk of tumor formation, although this is extremely rare.
Are there any age restrictions or limitations on who can undergo stem cell therapy for avascular necrosis of the hip?
There are typically no strict age restrictions for stem cell therapy in avascular necrosis. However, candidacy depends more on the patient’s overall health status, severity of the condition, and response to other treatments rather than age alone.
How effective is stem cell therapy compared to other treatments for avascular necrosis of the hip, such as core decompression or total hip replacement?
Stem cell therapy has shown promising results in promoting bone regeneration and reducing symptoms in early stages of avascular necrosis. Compared to other treatments, it may offer a less invasive option with the potential to delay or avoid the need for total hip replacement.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]