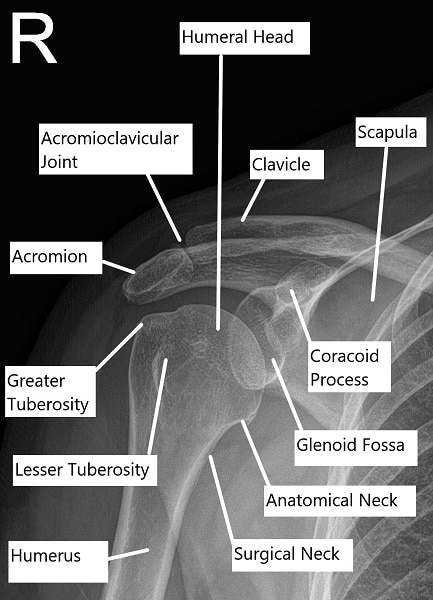
How the Body Part Normally Works? (Relevant Anatomy)
The shoulder is a highly mobile joint composed of the humerus (upper arm bone), scapula (shoulder blade), and clavicle (collarbone). The rotator cuff consists of four muscles: the supraspinatus, infraspinatus, teres minor, and subscapularis, which help stabilize the shoulder and allow for a wide range of motion. The subacromial space, located beneath the acromion, is where the rotator cuff tendons pass through. If this space becomes narrowed, it can lead to impingement, which causes pain and dysfunction.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with shoulder impingement syndrome commonly experience:
-
Pain: Especially on the front and side of the shoulder, worsened by overhead activities.
-
Weakness: Difficulty lifting objects or raising the arm overhead.
-
Limited Motion: Reduced ability to rotate or move the arm freely.
-
Night Pain: Waking up due to shoulder discomfort, particularly when sleeping on the affected side.
-
Tenderness: Notable sensitivity over the front of the shoulder or around the acromion.
How Doctors Find the Problem? (Diagnosis and Imaging)
A physician will conduct a thorough physical examination, checking for tenderness, weakness, and range of motion. Several tests, such as the Neer Impingement Test or Hawkins-Kennedy Test, are used to provoke symptoms and confirm the diagnosis.
Imaging studies are crucial for diagnosis:
-
X-rays: Used to assess bone spurs or other bony changes that might be causing the impingement.
-
MRI: Provides detailed images of the soft tissues, including the rotator cuff tendons and bursa, confirming the presence of impingement or tears.
Classification
Shoulder impingement can be classified into two main types:
-
Primary Impingement: Caused by anatomical changes, such as bone spurs or a hooked acromion.
-
Secondary Impingement: Often due to instability of the shoulder joint, which leads to abnormal movement and compression of the tendons.
Other Problems That Can Feel Similar (Differential Diagnosis)
Several conditions can mimic the symptoms of shoulder impingement, including:
Treatment Options
Non-Surgical Care
Initial treatment for impingement syndrome focuses on reducing pain and inflammation:
-
Rest and Ice: To reduce swelling and alleviate discomfort.
-
NSAIDs: Nonsteroidal anti-inflammatory drugs to reduce pain and inflammation.
-
Physical Therapy: Focused on strengthening the rotator cuff muscles and improving flexibility.
-
Cortisone Injections: These can reduce inflammation and provide relief in cases that are not improving with other treatments.
Surgical Care
When conservative treatments fail, surgery may be required. Arthroscopic surgery is the most common approach:
-
Subacromial Decompression (SAD): This procedure removes bone spurs and any inflamed tissue to create more space in the subacromial area.
-
Bursectomy: Removal of the inflamed bursa to relieve irritation.
-
Distal Clavicle Excision (DCE): If bone spurs on the clavicle are contributing to the impingement, they may be removed.
Postoperative Care and Rehabilitation
After surgery, patients are typically placed in a sling for a few weeks to minimize shoulder movement.
-
Physical Therapy: Gradual rehabilitation starts 1–4 weeks after surgery to restore range of motion and strength.
-
Recovery: Most patients can return to normal activities within 6–8 weeks, although it may take longer for high-impact or overhead activities.
Possible Risks and Complications (Complications)
While complications are rare, they can include:
-
Infection: Can usually be managed with antibiotics.
-
Stiffness: Shoulder stiffness may occur, which can be treated with physical therapy.
-
Recurrent Impingement: In some cases, symptoms may return, requiring further treatment.
-
Damage to Nerves or Blood Vessels: Rare but can occur during surgery.
Long-Term Outlook (Prognosis)
The prognosis after treatment for shoulder impingement is generally good, especially with early intervention. Most patients experience significant pain relief and regain normal shoulder function within 3–6 months. However, full recovery depends on the extent of the impingement and the individual’s adherence to postoperative rehabilitation.
Out-of-Pocket Costs
Medicare
CPT Code 29826 – Subacromial Decompression and Bursectomy: $40.07
CPT Code 29824 – Subacromial Decompression with DCE (Distal Clavicle Excision): $161.54
Medicare Part B typically covers 80% of the approved cost for these procedures once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce patient costs.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans typically cover any remaining coinsurance or small deductibles, which generally range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your subacromial decompression or bursectomy is required due to a work-related injury, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your shoulder condition requiring decompression surgery is linked to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
John Roberts required subacromial decompression and bursectomy (CPT 29826) to address chronic shoulder impingement. His estimated Medicare out-of-pocket cost was $40.07. Since John had supplemental insurance through Blue Cross Blue Shield, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. What is shoulder impingement syndrome?
A. Shoulder impingement syndrome occurs when the tendons of the rotator cuff are pinched or irritated due to narrowing of the subacromial space.
Q. How is shoulder impingement treated?
A. Treatment may begin conservatively with rest, ice, NSAIDs, and physical therapy. If symptoms persist, surgery such as subacromial decompression may be necessary.
Q. How long is the recovery after shoulder impingement surgery?
A. Recovery typically takes 3–6 months, with most patients returning to normal activities within 6–8 weeks.
Q. What are the risks of surgery for shoulder impingement?
A. Risks include infection, stiffness, recurrence of symptoms, and damage to nerves or blood vessels.
Summary and Takeaway
Shoulder impingement syndrome is a common and treatable condition. Conservative treatments are effective for many individuals, but surgical intervention may be needed for persistent or severe cases. With early diagnosis and appropriate treatment, patients can expect significant relief from pain and recovery of shoulder function.
Clinical Insight & Recent Findings
A recent study introduced a smart physical activity monitoring system to prevent Shoulder Impingement Syndrome (SIS) using wearable sensors and machine learning.
This innovative system monitors shoulder movements through gyroscopes and accelerometers, detecting deviations from normal movement patterns that could indicate impingement risk. The study demonstrated the system’s ability to predict SIS with high accuracy—88% for the Neural Network model—by analyzing sensor data and providing real-time feedback to adjust movements.
The results suggest that integrating wearable sensors with machine learning can offer personalized, proactive interventions, making it a significant advancement in SIS prevention. (“Study on Shoulder Impingement Syndrome – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons, especially those specializing in shoulder surgery, perform treatments for shoulder impingement syndrome.
When to See a Specialist?
Consult a specialist if you have persistent shoulder pain, difficulty lifting, or reduced range of motion despite conservative treatment.
When to Go to the Emergency Room?
Seek emergency care if you experience severe shoulder pain, sudden loss of function, or signs of infection (e.g., fever, redness, pus).
What Recovery Really Looks Like?
Recovery involves physical therapy and gradual return to activity, with most patients experiencing pain relief and improved shoulder function within a few months.
What Happens If You Ignore It?
Ignoring shoulder impingement can lead to worsening symptoms, including weakness, limited motion, and potential tears in the rotator cuff.
How to Prevent It?
Regular strengthening exercises for the shoulder, avoiding repetitive overhead movements, and proper posture can help prevent impingement syndrome.
Nutrition and Bone or Joint Health
A healthy diet rich in protein, calcium, and vitamin D supports tendon and bone health. Avoid smoking, as it can impair healing.
Activity and Lifestyle Modifications
After recovery, regular shoulder exercises and avoiding repetitive strain can help prevent recurrence of impingement syndrome.