Facet Joint Syndrome
Facet Joint Syndrome is a condition caused by wear and tear of the small joints located along the back of the spine. These joints, called facet joints, allow the vertebrae to glide smoothly during movement. When the joints become inflamed or their protective cartilage wears away, they can cause neck or lower-back pain that may radiate to nearby areas.
How Common It Is and Who Gets It? (Epidemiology)
Facet joint problems are common in adults over the age of 40 and increase with age. The lumbar (lower back) and cervical (neck) areas are affected most often. People who perform repetitive bending, twisting, or heavy lifting are more likely to develop this condition. Women, smokers, and those with obesity or prior spine injuries have slightly higher risk.
Why It Happens – Causes (Etiology and Pathophysiology)
Facet joint syndrome develops when the articular cartilage covering the ends of the facet bones wears away, leading to friction, inflammation, and pain.
Key causes include:
-
Age-related degeneration: Natural loss of cartilage and joint fluid.
-
Disc height loss: When spinal discs shrink, they shift more load onto the facet joints.
-
Repetitive strain: Frequent bending or twisting, common in athletes or laborers.
-
Trauma: Sudden impact or whiplash injuries.
-
Arthritis: Osteoarthritis can accelerate degeneration and cause bone spurs that narrow the joint space.
As degeneration progresses, the joints may enlarge, stiffen, or compress nearby nerves.
How the Body Part Normally Works? (Relevant Anatomy)
Each vertebra has two pairs of facet joints—one connecting to the vertebra above and one to the vertebra below. They act as hinges, guiding spinal motion while preventing excessive twisting.
The joint surfaces are lined with cartilage and surrounded by a capsule that produces synovial fluid, keeping the joint lubricated. When cartilage thins or the capsule becomes inflamed, the smooth motion is lost and pain signals are sent through tiny medial branch nerves.
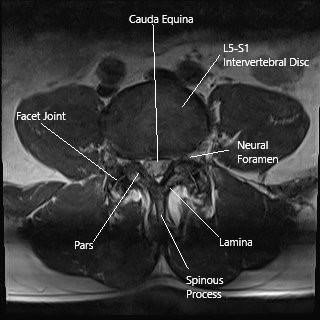
Axial section of the lumbar spine showing the facet joints.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms vary depending on the location of the affected joints:
-
Lumbar (lower back): Dull aching pain in the lower back, buttocks, or upper thighs. Pain often worsens after inactivity and improves with gentle movement or bending forward.
-
Cervical (neck): Aching pain in the neck, shoulders, or upper back. Pain may worsen with turning or tilting the head.
Other possible symptoms include stiffness, tenderness over the affected area, and, when nerve roots are irritated, shooting pain into the arm or leg (radiculopathy).
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed medical history and physical exam to determine where the pain originates.
Tests may include:
-
X-rays: Reveal bone spurs and joint alignment.
-
MRI: Shows inflammation and nerve involvement.
-
CT scans: Provide detailed images of bone and joint structure.
-
Diagnostic facet injections: A numbing and steroid injection into the joint or surrounding nerves. If pain relief follows, the joint is confirmed as the pain source.
Classification
Facet joint disease can be described by region (cervical, thoracic, lumbar) and stage:
-
Early: Mild inflammation and occasional stiffness.
-
Moderate: Joint cartilage loss with more frequent pain.
-
Advanced: Bone spurs and nerve compression causing chronic pain or referred symptoms.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may resemble facet joint syndrome include:
-
Herniated or bulging discs
-
Sacroiliac joint dysfunction
-
Spinal stenosis
-
Muscle strain or ligament sprain
-
Arthritis or ankylosing spondylitis
Imaging and diagnostic injections help distinguish between these causes.
Treatment Options
Non-Surgical Care
Most patients improve with conservative treatment:
-
Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants for pain control.
-
Physical therapy: Focuses on posture correction, flexibility, and strengthening core muscles to support the spine.
-
Heat or cold therapy: Reduces inflammation and muscle tension.
-
Lifestyle changes: Weight management, ergonomic adjustments, and avoiding repetitive bending.
-
Facet injections: Corticosteroid and anesthetic injections can reduce inflammation and pain for weeks or months.
Surgical Care
Surgery is rarely needed but may be considered if non-surgical options fail.
-
Radiofrequency ablation (RFA): Uses heat to disable the small medial branch nerves that carry pain signals from the facet joint.
-
Spinal fusion: In severe cases with instability, adjacent vertebrae are permanently joined to prevent painful movement.
Recovery and What to Expect After Treatment
Most patients notice gradual improvement over several weeks with therapy and medication. After RFA or injections, pain relief may last from six months to two years. Following spinal fusion, recovery takes several months with physical therapy to restore mobility and strength.
Possible Risks or Side Effects (Complications)
Risks are uncommon but can include:
-
Temporary soreness after injections
-
Infection or bleeding at the injection site
-
Nerve irritation or allergic reaction to medications
-
Persistent pain requiring additional treatment
Surgical risks include infection, hardware failure, or stiffness at the fused level.
Long-Term Outlook (Prognosis)
The prognosis is generally excellent. Many patients regain full activity with therapy, posture correction, and healthy habits. However, degeneration can progress with age, requiring periodic treatment for flare-ups.
Out-of-Pocket Costs
Medicare
CPT Code 64490 – Facet Injection (Cervical/Thoracic): $43.90
CPT Code 64493 – Facet Injection (Lumbar/Sacral): $40.70
CPT Code 64633 – Radiofrequency Ablation (RFA) / Neurotomy (Cervical/Thoracic): $98.54
CPT Code 64635 – Radiofrequency Ablation (RFA) / Neurotomy (Lumbar/Sacral): $99.35
Under Medicare, patients are responsible for 20% of the approved cost for each procedure once the annual deductible has been met. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover this 20%, eliminating or significantly reducing out-of-pocket expenses for Medicare-approved facet joint procedures. These supplemental policies work in conjunction with Medicare to close the cost gap for both diagnostic and therapeutic spinal interventions.
Secondary insurance—such as Employer-Based Plans, TRICARE, or Veterans Health Administration (VHA)—acts as a secondary payer after Medicare processes the claim. Once the deductible is met, secondary insurance may cover the remaining coinsurance or balance. These plans sometimes have their own deductible, typically ranging between $100 and $300, depending on the policy and whether services are rendered by in-network providers.
Workers’ Compensation
If your facet joint pain is the result of a work-related injury or repetitive strain, Workers’ Compensation will fully cover all diagnostic and treatment-related costs, including facet joint injections or radiofrequency ablation. Under Workers’ Compensation, you will not have any out-of-pocket expenses for approved care.
No-Fault Insurance
If your facet joint pain was caused or aggravated by a motor vehicle accident, No-Fault Insurance will pay for all necessary medical and interventional procedures, such as facet injections and radiofrequency ablation. The only possible charge is a small deductible depending on your specific policy details.
Example
Patricia, a 63-year-old patient, underwent lumbar facet joint injections (CPT 64493) followed by radiofrequency ablation (CPT 64635) to treat chronic low back pain from facet joint syndrome. Her Medicare out-of-pocket costs were $40.70 and $99.35, respectively. Because she had supplemental insurance through AARP Medigap, the remaining 20% that Medicare did not cover was fully paid, resulting in no out-of-pocket expense for her procedures.
Frequently Asked Questions (FAQ)
Q. Is facet joint syndrome the same as arthritis?
A. Yes, it is a type of spinal arthritis affecting the small joints between vertebrae.
Q. How long do injections last?
A. Relief varies, but many patients experience several months of pain reduction.
Q. Can exercise help?
A. Yes. Strengthening the back and abdominal muscles stabilizes the spine and reduces stress on the joints.
Q. Will I need surgery?
A. Surgery is rare and only considered if other treatments fail.
Summary and Takeaway
Facet joint syndrome occurs when the small stabilizing joints of the spine become worn or inflamed, leading to back or neck pain. Most patients improve with physical therapy, medication, and targeted injections. Long-term relief is possible with posture correction, exercise, and healthy lifestyle choices.
Clinical Insight & Recent Findings
A recent prospective study investigated the use of platelet-rich plasma (PRP) injections for treating chronic lumbar facet joint syndrome and compared it with local anesthetic injections. In the trial involving 78 patients, those who received CT-guided PRP injections showed significantly greater pain reduction and functional improvement than those treated with anesthetics alone.
Pain scores in the PRP group dropped by more than half within six weeks and remained low for up to one year, while the anesthetic group’s pain relief diminished after six months. Similarly, the Oswestry Disability Index—used to measure mobility and daily function—improved by nearly 50% in the PRP group, indicating lasting benefit.
The study attributed these effects to PRP’s biological action, which promotes tissue repair and reduces inflammation without the side effects associated with steroids or cortisone. These findings suggest PRP injections may offer a safe and long-term treatment option for patients with facet joint syndrome. (Study of PRP therapy for lumbar facet joint syndrome – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is managed by orthopedic spine surgeons, pain management physicians, and physical therapists, often working together to provide both non-surgical and interventional care.
When to See a Specialist?
You should see a specialist if you have:
-
Chronic back or neck pain lasting more than a few weeks
-
Pain that worsens when twisting or extending the spine
-
Pain relief when leaning forward or resting
When to Go to the Emergency Room?
Go to the ER if you experience:
-
Sudden weakness or numbness in the arms or legs
-
Loss of bladder or bowel control
-
Severe, unexplained pain after an injury
What Recovery Really Looks Like?
Most people resume normal activities within days after injections or RFA. Physical therapy continues to build flexibility and strength. For chronic cases, periodic treatment keeps symptoms under control.
What Happens If You Ignore It?
Without treatment, pain and stiffness may worsen over time. In severe cases, bone spurs or joint swelling can press on nerves, causing chronic pain or limited mobility.
How to Prevent It?
-
Maintain good posture during work and rest.
-
Exercise regularly to keep back and core muscles strong.
-
Avoid repetitive twisting and heavy lifting.
-
Keep a healthy weight to reduce spinal stress.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and omega-3 fatty acids supports bone and joint health. Staying hydrated and avoiding smoking help maintain healthy cartilage.
Activity and Lifestyle Modifications
Low-impact activities such as swimming, yoga, or walking improve flexibility and spinal stability. Ergonomic adjustments at work and frequent stretching reduce strain on the spine.
Do you have more questions?
What exactly are facet joints and their function?
Facet joints are small synovial joints located between and behind adjacent vertebrae in the spine. They provide stability and help guide motion, allowing for flexion, extension, and rotation of the spine. These joints are critical for maintaining the spine’s flexibility while preventing excessive movement that could damage the spinal cord and nerves.
How does Facet Joint Syndrome develop?
Facet Joint Syndrome develops primarily due to degenerative changes in the facet joints, often from aging. The cartilage in the joints wears down, leading to arthritis and inflammation. Injury, repetitive stress, poor posture, obesity, and genetic predispositions can also contribute to its development.
What are the main symptoms of Facet Joint Syndrome?
The main symptoms include:
- Localized pain in the lower back, middle back, or neck.
- Radiating pain to the buttocks, thighs, or shoulders.
- Stiffness and reduced mobility, particularly after inactivity.
- Tenderness around the affected joints.
- Increased pain with movement, such as twisting, bending, or lifting.
How is Facet Joint Syndrome diagnosed?
Diagnosis involves:
- Medical history and physical examination to assess pain points and mobility.
- Imaging studies like X-rays, MRI, or CT scans to visualize joint degeneration.
- Diagnostic injections where a local anesthetic is injected into the joint; relief from this injection confirms the facet joint as the pain source.
What non-surgical treatments are available for Facet Joint Syndrome?
Non-surgical treatments include:
- Medications such as pain relievers and muscle relaxants.
- Physical therapy with exercises to strengthen and stretch supporting muscles.
- Interventional procedures like facet joint injections and radiofrequency ablation.
- Lifestyle modifications including weight management and posture improvement.
How effective are facet joint injections?
Facet joint injections, typically containing steroids, can be very effective in reducing inflammation and pain. They provide temporary relief, which can last from several weeks to months. This procedure is often used when other conservative treatments have not been effective.
What is radiofrequency ablation and how does it help?
Radiofrequency ablation uses heat generated by radio waves to disrupt the nerve supply to the painful facet joint. This procedure can provide longer-term pain relief, often lasting from 6 months to 2 years, by effectively “turning off” the pain signals from the affected joint.
When is surgery considered for Facet Joint Syndrome?
Surgery is considered when conservative treatments fail to provide relief. Procedures like spinal fusion or facet joint replacement may be performed to stabilize the spine and alleviate pain by addressing the structural issues in the joints.
Can Facet Joint Syndrome be prevented?
While it can’t always be prevented, you can reduce the risk by maintaining a healthy weight, practicing good posture, engaging in regular exercise, and using proper techniques when lifting objects to avoid injury.
Is Facet Joint Syndrome a chronic condition?
Yes, it can be a chronic condition. However, with appropriate management, including medical treatments, physical therapy, and lifestyle modifications, many patients can control their symptoms effectively and maintain a good quality of life.
Are there any specific exercises recommended for Facet Joint Syndrome?
Exercises that strengthen the core muscles and improve flexibility are recommended. Low-impact activities like swimming, walking, and yoga can be beneficial. It’s best to work with a physical therapist to develop a tailored exercise program.
How do weight and obesity affect Facet Joint Syndrome?
Excess weight increases the load on the spine, accelerating the wear and tear on the facet joints. Managing weight through a healthy diet and regular exercise can reduce the strain on the spine and alleviate symptoms.
How long does it take to see improvements with treatment?
The time frame for improvement varies. Some patients may see relief within a few weeks of starting treatment, while others may take longer. Consistent adherence to treatment plans, including physical therapy and lifestyle modifications, is essential for optimal results.
What role does physical therapy play in managing Facet Joint Syndrome?
Physical therapy plays a crucial role by:
- Improving spinal stability and flexibility.
- Reducing muscle tension and pain.
- Teaching proper body mechanics and posture.
- Providing personalized exercise programs to strengthen supporting muscles.
Can poor posture alone cause Facet Joint Syndrome?
While poor posture alone may not directly cause Facet Joint Syndrome, it can contribute significantly to the condition by placing undue stress on the spine and facet joints, accelerating degenerative changes.
What are the potential side effects of facet joint injections?
Potential side effects include:
- Temporary increase in pain at the injection site.
- Infection.
- Bleeding.
- Allergic reactions to the injected substances.
- Nerve damage, though rare.
How often can I receive facet joint injections?
Facet joint injections can be administered several times a year, depending on the patient’s response and pain levels. Typically, injections are spaced out by at least a few months to prevent overuse of steroids and potential side effects.
Are there any alternative therapies for Facet Joint Syndrome?
Alternative therapies may include:
- Acupuncture.
- Chiropractic care.
- Massage therapy.
- Mind-body techniques like yoga and meditation.
These therapies can complement conventional treatments but should be discussed with a healthcare provider.
How does aging affect the facet joints?
Aging leads to the degeneration of cartilage in the facet joints, resulting in arthritis. The joints lose their smooth surface, causing pain and inflammation. Aging also leads to decreased flexibility and strength, contributing to joint stress.
Is Facet Joint Syndrome the same as arthritis?
Facet Joint Syndrome is a type of arthritis affecting the facet joints in the spine. It involves similar degenerative processes and symptoms, including pain and stiffness, as seen in other types of arthritis.
Can children or adolescents develop Facet Joint Syndrome?
While rare, children and adolescents can develop Facet Joint Syndrome, typically due to trauma or congenital abnormalities. It is more commonly seen in adults due to degenerative changes.
What dietary changes can help manage Facet Joint Syndrome?
A diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can help manage inflammation. Avoiding processed foods, excessive sugar, and unhealthy fats is also beneficial.
How do I know if my back pain is from Facet Joint Syndrome or another condition?
A thorough evaluation by a healthcare provider, including a physical exam, imaging studies, and possibly diagnostic injections, is necessary to determine if back pain is from Facet Joint Syndrome or another condition, such as a herniated disc or spinal stenosis.
Can facet joint problems lead to other complications?
If left untreated, Facet Joint Syndrome can lead to chronic pain and reduced mobility. Severe degeneration can cause spinal instability and may contribute to the development of other conditions like spinal stenosis or spondylolisthesis.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
