Prolapsed Intervertebral Disk (PIVD)
Prolapsed Intervertebral Disc (PIVD)—also called a herniated or slipped disc—occurs when the soft inner material of a spinal disc pushes through a tear in its outer layer. This can press on nearby nerves or the spinal cord, leading to pain, numbness, or weakness. PIVD most often affects the lower back (lumbar spine) or the neck (cervical spine).
How Common It Is and Who Gets It? (Epidemiology)
Disc herniation is one of the most common causes of back and neck pain in adults between 30 and 50 years of age. Men are slightly more affected than women. It is most frequent in people who perform repetitive lifting, bending, or twisting, and in those who sit for long periods. Smoking, obesity, and poor posture also increase the risk.
Why It Happens – Causes (Etiology and Pathophysiology)
Each spinal disc acts as a cushion between vertebrae, absorbing shock and allowing smooth movement. With age, discs lose water content, becoming less flexible and more prone to tearing.
Common causes include:
-
Age-related degeneration (most common)
-
Repetitive motion or heavy lifting
-
Sudden twisting or trauma
-
Obesity or poor posture
-
Genetic predisposition
When the disc’s inner gel-like material (nucleus pulposus) escapes through the tough outer ring (annulus fibrosus), it can compress a nerve, leading to pain and inflammation.
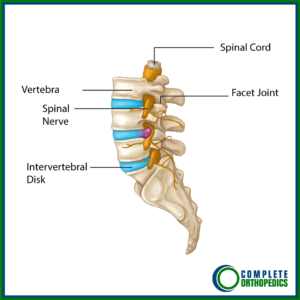
How the Body Part Normally Works? (Relevant Anatomy)
The intervertebral disc consists of three parts:
-
Annulus fibrosus: A tough, fibrous outer layer.
-
Nucleus pulposus: A soft, gel-like center that absorbs shock.
-
Endplates: Thin cartilage layers attaching the disc to the vertebrae.
Discs separate and cushion the vertebrae while allowing movement. When a disc prolapses or herniates, the displaced material can irritate or compress nerve roots within the spinal canal, causing pain and neurological symptoms.
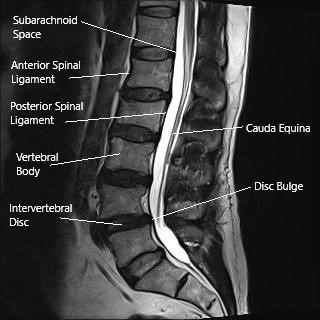
MRI of the lumbar spine in the sagittal section showing disc bulge.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms depend on the location and severity of nerve compression:
-
Lumbar (lower back) PIVD:
-
Lower back pain
-
Pain radiating down one or both legs (sciatica)
-
Numbness, tingling, or weakness in the legs or feet
-
-
Cervical (neck) PIVD:
-
Neck pain radiating to the shoulders, arms, or hands
-
Tingling or weakness in the arms or hands
-
-
Severe cases (Cauda Equina Syndrome):
-
Loss of bladder or bowel control
-
Numbness in the saddle area
-
Leg weakness or paralysis
This is a surgical emergency requiring immediate attention.
-
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis starts with a full medical history and physical examination to assess reflexes, strength, and sensation.
Imaging tests help confirm the diagnosis:
-
X-rays: Rule out other causes of back pain.
-
MRI: Shows disc herniation and nerve compression.
-
CT scan or myelogram: Used if MRI is not possible.
-
Electrodiagnostic studies (EMG/NCS): Assess nerve function if symptoms persist or are unclear.
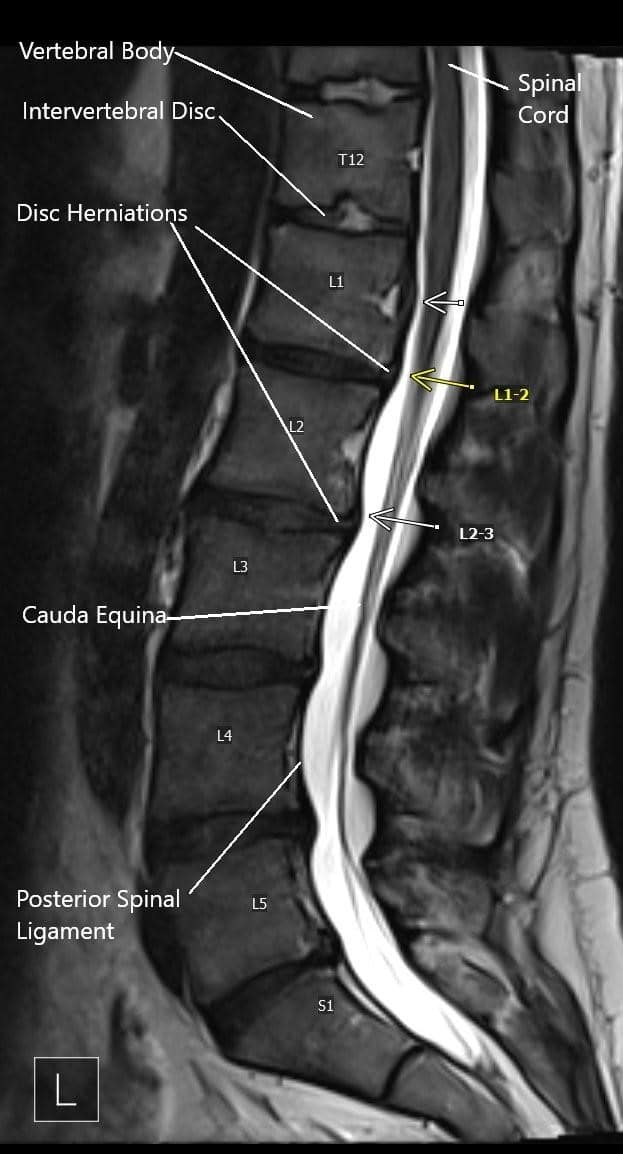
MRI image showing multiple disc herniations.
Classification
Herniated discs are classified based on anatomy and location:
By Anatomy:
-
Protrusion: Disc bulges outward but nucleus pulposus remains contained.
-
Extrusion: Nucleus pulposus breaks through the annulus fibrosus but remains attached to the disc.
-
Sequestration: Fragment separates completely from the disc.
By Location:
-
Central: Compresses spinal cord or cauda equina.
-
Paracentral: Most common; affects descending nerve roots.
-
Foraminal or far lateral: Compresses exiting nerve roots.
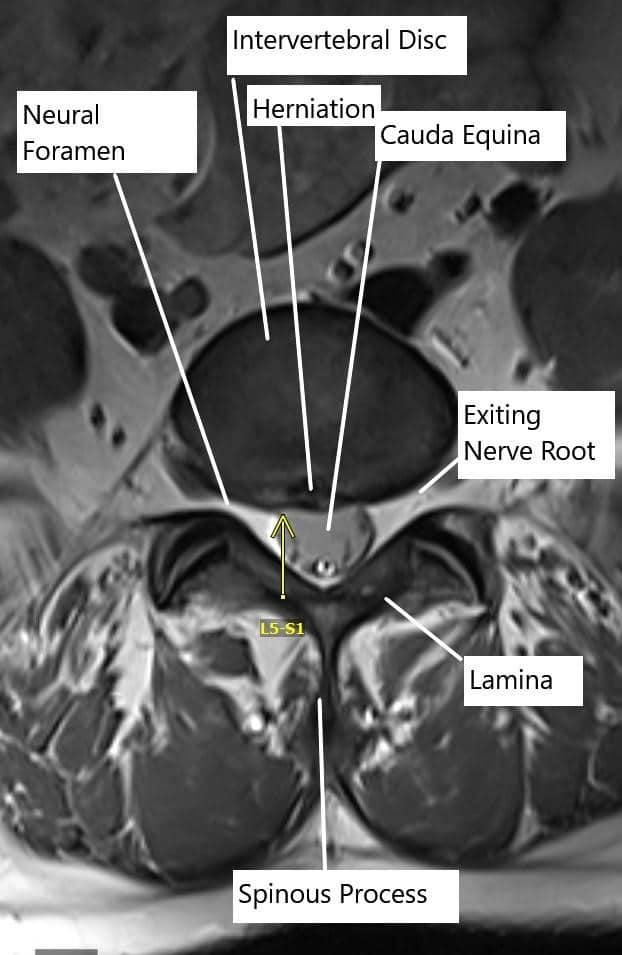
Axial section of the spine showing central disc herniation.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that mimic PIVD include:
-
Spinal stenosis
-
Spondylolisthesis (slipped vertebra)
-
Degenerative disc disease
-
Facet joint arthritis
-
Spinal tumors or infections
Treatment Options
Non-Surgical Care
Most patients improve without surgery.
Conservative management includes:
-
Rest and activity modification: Avoid lifting, twisting, or bending.
-
Medications: Anti-inflammatory drugs (NSAIDs), pain relievers, or muscle relaxants.
-
Heat and cold therapy: Ice for acute pain; heat for stiffness.
-
Physical therapy: Stretching and strengthening exercises once pain decreases.
-
Epidural steroid injections: Reduce inflammation and relieve nerve pain when conservative care isn’t enough.
Many herniated discs shrink naturally as the body reabsorbs the displaced material over several months.
Surgical Care
Surgery is considered when conservative measures fail or when neurological symptoms worsen.
Common procedures include:
-
Microdiscectomy: Minimally invasive removal of the herniated portion pressing on the nerve.
-
Laminectomy: Removal of part of the vertebral bone (lamina) to relieve pressure.
-
Discectomy with fusion: In cervical herniations, the disc is removed and the adjacent vertebrae are fused with bone graft and implants.
-
Artificial disc replacement: In selected cases, a motion-preserving alternative to fusion.
The goal of surgery is to relieve pressure on nerves, reduce pain, and restore function.
Recovery and What to Expect After Treatment
-
Non-surgical recovery: Symptoms usually improve within 6–12 weeks with rest and therapy.
-
Post-surgery: Most patients walk within hours and return home the same day or after one night. Full recovery takes 4–8 weeks, depending on activity level and procedure.
Physical therapy helps strengthen core muscles and prevent recurrence.
Possible Risks or Side Effects (Complications)
Complications are uncommon but may include:
-
Infection or bleeding
-
Nerve injury or numbness
-
Recurrence of disc herniation
-
Spinal fluid leakage (dural tear)
-
Persistent pain or stiffness
Following post-operative instructions reduces risk and improves healing.
Long-Term Outlook (Prognosis)
Most patients recover fully and return to normal activities. Pain relief is achieved in over 90% of surgical cases. Recurrence is rare if proper posture, exercise, and lifestyle changes are maintained.

Shavers used for removing intervertebral disc material

Instruments used for lumbar spinal fusion
The instruments in the image above are used to remove the intervertebral disc material, create raw surface for the insertion of the bone cage and insert the pedicle screws.
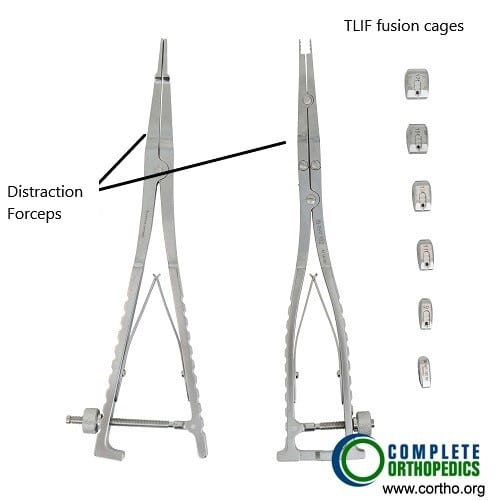
Distraction forceps and TLIF cages
The transforaminal lumbar interbody fusion (TLIF) utilizes a lateral incision from the back for fusion of the vertebrae. The image above shows distraction forceps used to create a space between the vertebra for insertion of the bone cage along with the bone graft material for aiding the fusion of the involved segment.
Out-of-Pocket Costs
Medicare
CPT Code 63075 – Cervical Discectomy: $333.20
CPT Code 63055 – Thoracic Discectomy: $403.73
CPT Code 63030 – Lumbar Discectomy / Microdiscectomy: $225.06
CPT Code 22558 – Anterior Lumbar Interbody Fusion (ALIF): $368.50
Under Medicare, 80% of the approved amount for these procedures is covered after the annual deductible has been met. The remaining 20% is the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—are designed to cover this coinsurance, significantly reducing or eliminating out-of-pocket costs for Medicare-approved spinal surgeries. These plans coordinate directly with Medicare, ensuring patients typically have full coverage for procedures such as discectomy or spinal fusion.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer after Medicare has processed the claim. Once your deductible is satisfied, the secondary plan may pay the remaining coinsurance and any balance due. Deductibles for secondary insurance plans usually range between $100 and $300, depending on your policy and network status.
Workers’ Compensation
If your PIVD developed or was aggravated due to work-related activities, Workers’ Compensation will cover the full cost of surgical treatment, including cervical, thoracic, or lumbar discectomy and spinal fusion if required. This includes all hospital, surgical, and postoperative expenses, leaving you with no out-of-pocket cost under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your disc herniation occurred as a result of an automobile accident, No-Fault Insurance will cover all medical and surgical costs associated with your diagnosis and treatment, including discectomy and fusion procedures. You may only be responsible for a small deductible depending on the details of your policy.
Example
Sonia, a 58-year-old patient, suffered from lumbar disc herniation causing leg pain and weakness. She underwent lumbar microdiscectomy (CPT 63030) with an estimated Medicare out-of-pocket cost of $225.06. Because she had supplemental insurance through AARP Medigap, the 20% coinsurance not paid by Medicare was fully covered, resulting in no out-of-pocket expense for her surgery.
Frequently Asked Questions (FAQ)
Q. Can a herniated disc heal on its own?
A. Yes. Many cases improve with time and conservative therapy as the body reabsorbs the herniated material.
Q. When is surgery necessary?
A. Surgery is recommended if pain lasts beyond 6–12 weeks despite therapy, or if there is leg weakness or loss of bladder/bowel control.
Q. Can physical therapy help prevent recurrence?
A. Yes. Strengthening the back and abdominal muscles reduces stress on the discs.
Q. Are injections a permanent solution?
A. No, but they can provide temporary relief to allow participation in therapy.
Summary and Takeaway
A prolapsed intervertebral disc occurs when the inner disc material presses on nearby nerves, causing back or neck pain and possible numbness or weakness. Most people recover with conservative care, but surgery can relieve persistent or severe nerve compression. Early diagnosis, lifestyle changes, and proper rehabilitation help ensure long-term recovery.
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is provided by orthopedic spine surgeons or neurosurgeons, supported by physical therapists, pain specialists, and rehabilitation experts.
When to See a Specialist?
See a specialist if you have:
-
Persistent back or neck pain
-
Numbness, tingling, or weakness in your arms or legs
-
Pain that worsens when sitting or bending
-
Difficulty walking or standing for long periods
When to Go to the Emergency Room?
Seek immediate medical care if you experience:
-
Sudden loss of bladder or bowel control
-
Severe leg weakness or paralysis
-
Numbness in the saddle area (buttocks, thighs, genitals)
These symptoms may indicate cauda equina syndrome, a surgical emergency.
What Recovery Really Looks Like?
Recovery is gradual. Pain improves first, followed by strength and flexibility. Physical therapy restores stability and confidence in movement. Most people return to work and normal activities within a few months.
What Happens If You Ignore It?
Untreated disc herniation can lead to chronic pain, nerve damage, or permanent weakness. In severe cases, compression can cause paralysis or loss of bladder control.
How to Prevent It?
-
Maintain good posture while sitting or lifting.
-
Avoid repetitive bending or twisting.
-
Exercise regularly to strengthen core muscles.
-
Maintain a healthy weight and avoid smoking.
Nutrition and Bone or Joint Health
A balanced diet rich in calcium, vitamin D, and protein supports spinal bone health. Staying hydrated keeps spinal discs flexible and resilient.
Activity and Lifestyle Modifications
Stay active with low-impact exercises like swimming, yoga, or walking. Use proper ergonomics at work, avoid long sitting periods, and lift objects using your legs, not your back.
For TLIF procedure and cost information, please click here.
Do you have more questions?
What is PIVD?
PIVD is a condition where the inner gel-like material of a spinal disc bulges or ruptures through its outer layer, compressing the spinal nerves and causing pain and other symptoms.
What are the common symptoms of PIVD?
Symptoms include lower back pain, radiating pain to the legs, numbness, tingling, and weakness in the legs. For cervical PIVD, symptoms include neck pain, shoulder pain, radiating pain to the arms, and weakness in the arms.
What causes PIVD?
PIVD can be caused by age-related degeneration, repetitive activities, improper posture, obesity, smoking, lifting heavy weights, or traumatic injuries.
How is PIVD diagnosed?
Diagnosis involves a detailed medical history, physical examination, and imaging tests such as MRI or CT scans to identify the location and severity of the herniation.
What is disc sequestration?
Disc sequestration occurs when the herniated nucleus pulposus loses contact with the original disc material and is free in the spinal canal.
What is the difference between a protrusion and extrusion in PIVD?
Protrusion means the nucleus pulposus bulges out but is still covered by a thin layer of annulus fibrosis. Extrusion means the nucleus pulposus breaks through the annulus but remains connected to the disc.
Can PIVD heal on its own?
Yes, many cases of PIVD can improve over time with conservative treatment as the herniated material may be reabsorbed by the body.
What conservative treatments are available for PIVD?
Conservative treatments include rest, physical therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and heat/cold therapy.
When is surgery needed for PIVD?
Surgery is considered if conservative treatments fail to relieve symptoms, if there is significant nerve compression causing severe pain or weakness, or in emergencies like cauda equina syndrome.
What is Microdiskectomy?
Microdiskectomy is a minimally invasive surgery to remove herniated disc material and relieve nerve compression. It involves a small incision and the use of a microscope
What are the risks of PIVD surgery?
Risks include infection, bleeding, nerve damage, spinal fluid leak, and incomplete relief of symptoms.
What is spinal fusion surgery?
Spinal fusion involves removing the herniated disc and fusing two adjacent vertebrae with bone grafts and hardware to stabilize the spine.
How long is the recovery after PIVD surgery?
Recovery varies but typically involves several weeks of limited activity followed by physical therapy. Full recovery can take several months.
What lifestyle changes can help prevent PIVD?
Maintaining a healthy weight, practicing good posture, avoiding smoking, and performing regular exercises to strengthen the back and abdominal muscles can help prevent PIVD.
Can PIVD recur after treatment?
Yes, there is a risk of recurrence, especially if underlying factors like poor posture or repetitive strain are not addressed.
What exercises are recommended for PIVD?
Low-impact activities like walking, swimming, and specific stretching and strengthening exercises for the core muscles are recommended.
Can physical therapy help with PIVD?
Yes, physical therapy can help alleviate symptoms, improve mobility, and strengthen the muscles supporting the spine.
Are there any alternative treatments for PIVD?
Some patients find relief with chiropractic care, acupuncture, or massage therapy, but these should be considered complementary to conventional treatments.
How can I manage pain from PIVD at home?
Pain can be managed with over-the-counter pain relievers, alternating heat and cold therapy, and avoiding activities that exacerbate the pain.
Is it safe to exercise with PIVD?
Yes, but exercises should be low-impact and approved by your healthcare provider to avoid aggravating the condition.
What is cauda equina syndrome?
Cauda equina syndrome is a medical emergency caused by severe compression of the nerve roots below the L1-L2 level, leading to loss of bowel/bladder control and numbness in the saddle area.
What should I do if I suspect cauda equina syndrome?
Seek immediate medical attention as it requires urgent surgical intervention to prevent permanent damage.
Can PIVD cause permanent nerve damage?
If left untreated or if severe, PIVD can cause permanent nerve damage resulting in chronic pain, numbness, or weakness.
How does smoking affect PIVD?
Smoking decreases blood supply to the discs, accelerating degeneration and increasing the risk of PIVD.
Can weight loss help with PIVD symptoms?
Yes, losing excess weight can reduce the strain on the spine and alleviate PIVD symptoms.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
