Spine Tumors
Spine tumors are abnormal growths of tissue that develop within or around the spinal cord and vertebral column. These growths occur when normal cells multiply uncontrollably and fail to respond to the body’s natural growth controls.
Spinal tumors can be benign (noncancerous), low-grade malignant, or high-grade malignant (cancerous). Depending on their origin, they may start in the spine itself (primary tumors) or spread from another part of the body (metastatic or secondary tumors).
How Common It Is and Who Gets It? (Epidemiology)
Spine tumors are relatively rare, accounting for about 10–15% of all central nervous system tumors. They can affect both men and women of any age, though certain types are more common in specific age groups.
-
Primary spinal tumors are uncommon and may develop at any age.
-
Metastatic spinal tumors occur more often in adults, especially those with cancers of the breast, lung, or prostate.
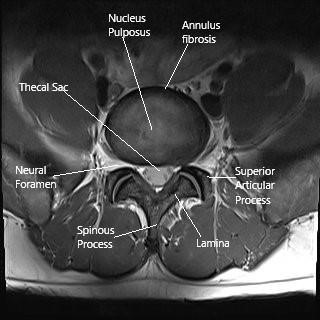
MRI of the lumbar spine in the axial section.
Why It Happens – Causes (Etiology and Pathophysiology)
The exact cause of spinal tumors is often unknown, but several factors may contribute:
-
Genetic mutations: Can trigger abnormal cell growth.
-
Inherited syndromes: Such as Neurofibromatosis Type 2 or Von Hippel–Lindau disease, which increase the risk of certain spinal tumors.
-
Metastatic spread: Cancer cells from other organs travel through the bloodstream or cerebrospinal fluid to the spine.
Tumor growth can compress the spinal cord and nerves, leading to pain, weakness, or even loss of function.
How the Body Part Normally Works? (Relevant Anatomy)
The spinal cord runs through the spinal canal, surrounded by protective layers called the meninges and the vertebrae. Nerves branch off from the spinal cord to transmit signals to the rest of the body.
When a tumor develops inside or near the spinal cord, it can compress these structures, leading to pain, numbness, weakness, and, in severe cases, loss of bowel or bladder control.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms vary depending on the tumor’s location, size, and growth rate but commonly include:
-
Persistent back pain that worsens at night or with movement
-
Radiating pain (sciatica-like pain) down the arms or legs
-
Numbness or tingling in the limbs
-
Weakness or loss of coordination
-
Bowel or bladder dysfunction
-
Difficulty walking or standing upright
-
In severe cases, paralysis below the affected level of the spine
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis involves a combination of medical history, neurological examination, and imaging tests:
-
X-rays: May reveal bone changes or structural damage.
-
MRI: The gold standard for detecting spinal cord and nerve compression, showing both soft tissue and bone detail.
-
CT scan: Provides detailed images of vertebrae and tumor invasion.
-
Bone scan or PET scan: Detects cancer spread (metastasis).
-
Biopsy: A small tissue sample confirms the tumor type and guides treatment.
Classification
Spine tumors are classified by location relative to the spinal cord:
-
Extradural tumors: Located outside the spinal cord’s protective covering (most metastatic tumors).
-
Intradural extramedullary tumors: Inside the spinal canal but outside the spinal cord tissue (commonly meningiomas and schwannomas).
-
Intradural intramedullary tumors: Inside the spinal cord tissue (commonly ependymomas and astrocytomas).
They can also be primary (originating in the spine) or secondary (spreading from another organ).
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic spinal tumors include:
-
Herniated disc or spinal stenosis
-
Spinal infections (osteomyelitis, abscess)
-
Multiple sclerosis or transverse myelitis
-
Vascular malformations
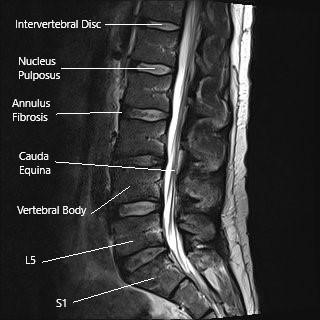
MRI of lumbar spine in sagittal section
Treatment Options
Non-Surgical Care
For small or slow-growing benign tumors, observation and regular MRI scans may be appropriate.
Other non-surgical treatments include:
-
Medications: Steroids to reduce inflammation and swelling.
-
Radiation therapy: To shrink tumors or kill remaining cancer cells after surgery.
-
Chemotherapy: Used primarily for malignant or metastatic tumors.
-
Targeted or immunotherapy: For specific cancers that spread to the spine.
Surgical Care
Surgery is often necessary when the tumor compresses the spinal cord or nerves, causing pain or neurological symptoms.
Surgical goals include:
-
Tumor removal or decompression of the spinal cord.
-
Spinal stabilization: Using rods, screws, or bone grafts if bone is removed during surgery.
-
Biopsy: To confirm tumor type before further therapy.
Minimally invasive techniques allow faster recovery and reduced surgical risks for select patients.
Recovery and What to Expect After Treatment
-
Post-surgery: Hospital stays typically range from 3–7 days.
-
Rehabilitation: Physical therapy helps restore strength and mobility.
-
Radiation or chemotherapy: May follow surgery to prevent recurrence.
Most patients experience significant relief from pain and improved function. Recovery time depends on tumor type, extent, and overall health.
Possible Risks or Side Effects (Complications)
Potential complications include:
-
Infection or bleeding
-
Nerve injury causing weakness or numbness
-
Spinal instability
-
Cerebrospinal fluid (CSF) leak
-
Recurrence or spread of cancer
Close follow-up and modern surgical techniques minimize these risks.
Long-Term Outlook (Prognosis)
The prognosis depends on tumor type, grade, and whether it is primary or metastatic.
-
Benign tumors: Often curable with complete surgical removal.
-
Malignant tumors: May be controlled with combined therapy (surgery, radiation, chemotherapy).
Early diagnosis and treatment are key to preserving spinal function and quality of life.
Out-of-Pocket Costs
Medicare
CPT Code 22842 – Spinal Stabilization (Instrumentation, 3–6 Segments): $185.26
CPT Code 22612 – Spinal Fusion (Posterior Lumbar, if needed): $382.85
CPT Code 20245 – Bone Biopsy (Deep, Spine or Pelvis): $79.16
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible is met. Patients are responsible for the remaining 20%. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, leaving most patients with no out-of-pocket costs for Medicare-approved procedures. These supplemental plans work seamlessly with Medicare, providing complete coverage for diagnostic and stabilizing spinal procedures like fusion, instrumentation, and biopsy.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer after Medicare has processed your claim. Once your deductible is satisfied, the secondary plan can pay any remaining balance, including coinsurance or small uncovered charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on your policy and provider network.
Workers’ Compensation
If your spinal instability or pathology requiring biopsy or stabilization is related to a work injury, Workers’ Compensation will pay for all medical and surgical expenses, including hardware placement and diagnostic biopsy. You will not have any out-of-pocket costs under an approved Workers’ Compensation claim.
No-Fault Insurance
If your spinal injury or condition was caused or worsened by a motor vehicle accident, No-Fault Insurance will cover all related diagnostic and surgical procedures, including stabilization, fusion, and biopsy. The only potential charge may be a small deductible depending on your policy terms.
Example
Michael, a 63-year-old patient, underwent spinal stabilization (CPT 22842) and bone biopsy (CPT 20245) after imaging showed spinal instability and a suspicious vertebral lesion. His Medicare out-of-pocket costs were $185.26 and $79.16, respectively. Because he had supplemental insurance through AARP Medigap, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for his procedures.
Frequently Asked Questions (FAQ)
Q. Are all spinal tumors cancerous?
A. No. Many spinal tumors, such as schwannomas or meningiomas, are benign and noncancerous. However, some are malignant or metastatic, spreading from other parts of the body.
Q. What are the warning signs of a spinal tumor?
A. Persistent back pain (especially at night), weakness, numbness, or loss of bladder/bowel control may indicate a spinal tumor and require prompt evaluation.
Q. How are spinal tumors treated?
A. Treatment depends on the tumor type and location. Options include surgery, radiation, chemotherapy, or a combination of these therapies.
Q. What is the recovery time after spinal tumor surgery?
A. Most patients recover in 6–12 weeks, though rehabilitation may continue longer for complex cases.
Summary and Takeaway
Spine tumors are abnormal growths within or around the spinal cord that can be benign or cancerous. Early diagnosis through MRI and biopsy is essential. Most patients benefit from surgical removal followed by radiation or chemotherapy, depending on the tumor type. Advances in microsurgery and imaging have made outcomes highly successful, improving pain relief, mobility, and overall quality of life.
Clinical Insight & Recent Findings
A recent review in the Global Spine Journal summarized major advances in radiotherapy for spinal tumors, emphasizing how stereotactic body radiation therapy (SBRT) and particle beam therapy (PBT) have transformed treatment outcomes. SBRT, which delivers high radiation doses in 1–5 sessions with precision targeting, achieved one-year local control rates of up to 94% for spinal metastases and provided superior pain relief compared with conventional radiotherapy.
The approach also reduced treatment-related side effects through smaller radiation margins and advanced image guidance. Particle therapies, including proton and carbon ion therapy, allow higher radiation doses to resistant primary tumors such as chordomas and chondrosarcomas while minimizing damage to nearby tissues. Five-year local control rates reached 78–80% with few major toxicities. The review also highlighted the integration of minimally invasive surgery and SBRT for complex metastatic cases, improving stability and postoperative recovery.
These findings underscore the importance of multidisciplinary, technology-driven treatment strategies to achieve durable tumor control, pain relief, and preservation of spinal function in patients with both primary and metastatic spine tumors. (Study of advanced radiotherapy and surgical strategies in spinal tumors – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is performed by orthopedic spine surgeons or neurosurgeons, with collaboration from oncologists, radiation specialists, pathologists, and rehabilitation teams.
When to See a Specialist?
You should see a spine specialist if you experience:
-
Persistent or worsening back pain not relieved by rest
-
Numbness, weakness, or tingling in the arms or legs
-
Difficulty walking or balancing
-
Loss of bladder or bowel control
When to Go to the Emergency Room?
Seek emergency care if you develop:
-
Sudden paralysis or severe leg weakness
-
Loss of sensation in the groin or buttocks
-
Inability to control urination or defecation (possible spinal cord compression)
What Recovery Really Looks Like?
Recovery depends on tumor type and treatment approach. Pain relief and improved strength are often noticed within weeks. Ongoing physical therapy enhances mobility and prevents complications.
What Happens If You Ignore It?
Untreated spinal tumors can cause permanent nerve damage, paralysis, or loss of bowel/bladder control. In malignant cases, ignoring symptoms allows cancer to spread and reduces survival chances.
How to Prevent It?
While most spinal tumors cannot be prevented, early detection through regular screening in patients with known cancers or genetic conditions helps identify lesions before symptoms occur.
Nutrition and Bone or Joint Health
A diet rich in protein, calcium, and vitamin D supports recovery and bone healing after surgery. Patients undergoing radiation or chemotherapy should maintain hydration and balanced nutrition to promote strength and immunity.
Activity and Lifestyle Modifications
After treatment, patients should avoid heavy lifting or twisting until cleared by their surgeon. Gradual activity resumption, guided by physical therapy, helps restore endurance and confidence.
Do you have more questions?
How common are spine tumors?
Primary spine tumors are rare, while metastatic spine tumors are more common, affecting up to 70% of cancer patients.
What types of spine tumors are most common?
The most common types of spine tumors are metastatic tumors. Among primary tumors, hemangiomas (benign vascular tumors) are common, followed by osteoid osteomas, osteoblastomas, and chondrosarcomas.
How are spine tumors diagnosed?
Diagnosis typically begins with imaging studies like X-rays, CT scans, or MRI. A biopsy may be performed to determine whether the tumor is benign or malignant and to guide treatment.
What is the prognosis for patients with spine tumors?
The prognosis depends on the type of tumor. Benign tumors generally have an excellent prognosis after surgical removal. The prognosis for metastatic tumors varies, depending on the type of primary cancer and how early the tumor is detected.
Can spine tumors be benign?
Yes, benign tumors like osteoid osteomas, osteoblastomas, and hemangiomas can occur in the spine. While non-cancerous, they may still cause symptoms and require treatment if they compress the spinal cord or nerves.
What role does MRI play in diagnosing spine tumors?
MRI is crucial for evaluating soft tissue structures, bone marrow involvement, and the relationship of the tumor to the spinal cord and nerves. It provides detailed information that helps in planning treatment.
Is surgery always necessary for spine tumors?
Surgery is often recommended for symptomatic spine tumors, especially if they cause neurological symptoms, spinal instability, or pain. However, for some benign tumors or tumors responding well to chemotherapy or radiation, surgery may not be necessary.
What are the surgical options for spine tumors?
Surgical options include tumor removal, spinal stabilization (with rods and screws), vertebroplasty (cement augmentation), and, in some cases, total en bloc spondylectomy (removal of an entire vertebra).
How are metastatic spine tumors treated?
Treatment for metastatic tumors often focuses on palliative care, including pain relief, radiation therapy, and surgery to stabilize the spine if necessary. Chemotherapy may be used depending on the type of primary cancer.
What is vertebroplasty, and when is it used?
Vertebroplasty involves injecting bone cement into the vertebra to stabilize it and relieve pain, often used in cases where the vertebra has weakened due to tumor growth or fracture.
Can spine tumors cause paralysis?
Yes, if a spine tumor compresses the spinal cord or nerves, it can lead to neurological deficits, including paralysis. Immediate treatment is crucial to prevent permanent damage.
What is the likelihood of a spine tumor recurring after surgery?
Recurrence depends on the type of tumor and how completely it was removed. Benign tumors like osteoid osteomas rarely recur if fully excised. Malignant tumors, however, may recur, particularly if not completely removed.
What is the role of radiation therapy in treating spine tumors?
Radiation therapy is used to shrink tumors, relieve pain, and improve neurological function. It is especially effective for metastatic tumors and some malignant primary tumors that are not amenable to surgery.
How can I tell if my back pain is from a spine tumor and not something else?
Back pain from spine tumors often has specific characteristics, such as worsening at night, being persistent despite rest, and being associated with other symptoms like numbness or weakness. Imaging studies are needed for a definitive diagnosis.
What is stereotactic radiosurgery, and how is it used for spine tumors?
Stereotactic radiosurgery is a precise form of radiation that delivers high doses of radiation directly to the tumor with minimal damage to surrounding tissues. It is often used for metastatic tumors and some primary tumors.
Can children develop spine tumors?
Yes, though rare, children can develop both benign and malignant spine tumors. Common pediatric spine tumors include osteoid osteomas, osteoblastomas, and Ewing’s sarcoma.
How do spine tumors affect mobility?
Spine tumors can impair mobility by causing pain, spinal instability, or neurological symptoms like weakness or paralysis. Treatment is aimed at relieving these symptoms and restoring mobility where possible.
Is there a genetic predisposition to developing spine tumors?
Some spine tumors, particularly primary tumors like chordoma, may have genetic links, but most occur sporadically without a known family history or genetic cause.
What happens if a spine tumor is left untreated?
If left untreated, spine tumors can grow, causing increased pain, spinal instability, and neurological deficits, including paralysis. Malignant tumors may metastasize to other areas of the body.
How are primary malignant spine tumors treated differently from metastatic tumors?
Primary malignant tumors are often treated with a combination of surgery (aiming for complete removal) and radiation or chemotherapy, depending on the type of cancer. Metastatic tumors typically focus on relieving symptoms, stabilizing the spine, and slowing tumor growth rather than aiming for a cure.
How long is the recovery period after surgery for spine tumors?
Recovery time depends on the type of surgery and the patient’s overall health. Minimally invasive procedures may require only a few weeks of recovery, while more extensive surgeries, like en bloc spondylectomy, may require several months.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
