Hip Replacement Surgery
Hip replacement is a surgical procedure designed to relieve pain and restore function for individuals suffering from severe hip arthritis or injury. The procedure involves replacing the damaged or worn-out components of the hip joint with artificial components that mimic the natural shape and function of the hip joint.
How Common It Is and Who Gets It? (Epidemiology)
Hip replacement surgery is a common and highly successful procedure, particularly among older adults, with over 300,000 procedures performed annually in the U.S. It is most commonly used to treat osteoarthritis, but it can also be performed for conditions like rheumatoid arthritis, hip fractures, and avascular necrosis. Hip replacement surgery is also becoming more common in younger, active patients with hip pain due to these conditions.
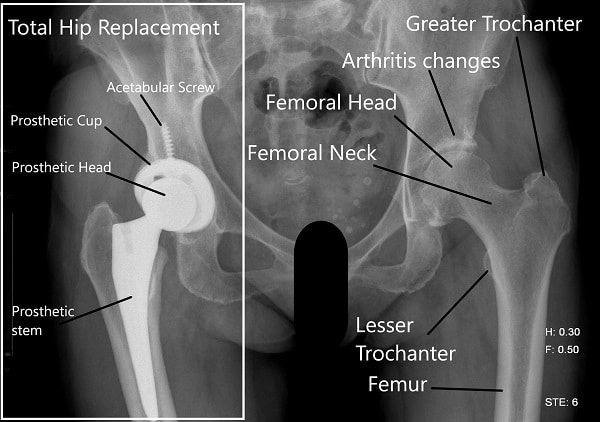
Hip x-ray
Materials and Equipment Used in Hip Replacement Surgery
The materials used for hip replacement are designed to provide durability and function for years. The key components include:
-
Femoral stem: Typically made from titanium, cobalt-chromium, or stainless steel. Some stems have porous coatings that allow bone ingrowth to help secure the implant.
-
Femoral head (ball): Usually made from ceramic or metal for durability and smooth movement.
-
Acetabular component: Often made of polyethylene (plastic), ceramic, or metal. The acetabular liner is the part that covers the hip socket and helps to prevent wear between the femoral head and the socket.
-
Cement: Some implants are fixed using bone cement, while others are press-fit, allowing the bone to grow into the implant over time.
-
Fluoroscopic imaging: Used during surgery for precise placement of the implant.
-
Retractors and surgical tools: Used for optimal exposure of the joint to facilitate the precise implantation of the artificial components.
These materials are designed for long-term durability and functionality, providing pain relief and improved mobility for patients undergoing hip replacement surgery.
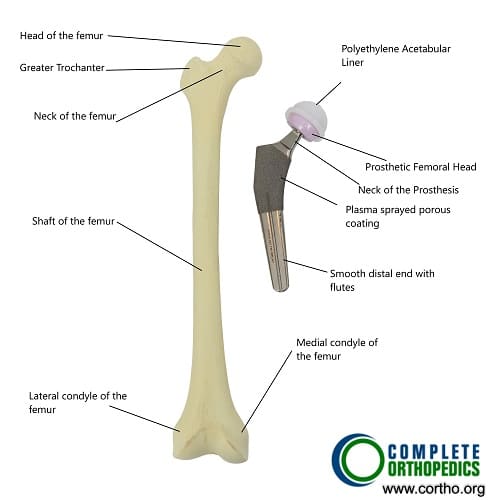
Total Hip Replacement Components
Why It Happens – Causes (Etiology and Pathophysiology)
The most common reason for hip replacement is osteoarthritis, a degenerative joint disease that leads to the gradual wearing away of the cartilage in the hip joint. Other causes include:
-
Rheumatoid arthritis, which causes inflammation of the joint lining.
-
Avascular necrosis, where the blood supply to the femoral head (the ball of the hip) is disrupted, leading to bone death and collapse.
-
Hip fractures, which can sometimes lead to the need for hip replacement if the fracture cannot be effectively repaired.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint made up of the femoral head (the ball) and the acetabulum (the socket in the pelvis). Healthy cartilage lines the joint surfaces, allowing for smooth, pain-free movement. The joint is stabilized by surrounding muscles, tendons, and ligaments, which help control and facilitate movement.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms that might indicate the need for hip replacement include:
-
Chronic pain in the hip, groin, thigh, or buttocks, which worsens with movement.
-
Stiffness and limited range of motion, especially when getting in or out of bed or a car.
-
Pain that worsens during walking, standing, or climbing stairs.
-
Difficulty performing daily activities such as standing, sitting, or bending down.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
Physical examination to assess hip range of motion, strength, and pain levels.
-
X-rays to evaluate joint space narrowing and bone damage.
-
MRI or CT scans for detailed images of soft tissues, cartilage, and bone damage.
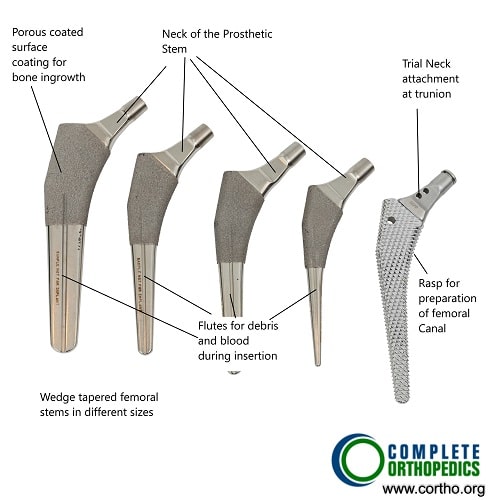
Different sizes of Femoral stems used for Primary Hip Replacement.
Procedure Types or Techniques (Classification)
Hip replacement surgery can be performed using different techniques:
-
Traditional hip replacement (posterior or lateral approach): Involves a larger incision and access through the back or side of the hip.
-
Minimally invasive hip replacement (anterior approach): Uses smaller incisions and causes less disruption to muscles and tendons, leading to quicker recovery.
-
Robot-assisted surgery: Allows for more precise placement of the implants and can help reduce recovery time.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that may mimic the symptoms of hip arthritis include:
-
Trochanteric bursitis (inflammation of the bursa near the hip).
-
Piriformis syndrome (sciatic nerve compression due to muscle spasms).
-
Hip labral tears (damage to the cartilage that forms the socket).
-
Lumbar radiculopathy (nerve irritation from the lower back).
Treatment Options
Before surgery, conservative treatments like physical therapy, medications (NSAIDs), and injections (corticosteroids) are typically tried. If these measures fail to alleviate pain or restore function, hip replacement surgery is recommended.
Recovery and What to Expect After Surgery
-
Post-operative care includes wearing a sling or immobilizer for the first 2–4 weeks to protect the hip while it heals.
-
Physical therapy begins within the first few days to regain movement, strength, and mobility.
-
Most patients experience pain relief and significant improvement in mobility within 6–12 weeks, with full recovery taking 6–12 months.
Possible Risks or Side Effects (Complications)
Although complications are rare, they can include:
-
Infection, blood clots, and nerve damage.
-
Dislocation of the artificial hip joint.
-
Leg length discrepancy, where one leg may be slightly longer or shorter than the other.
-
Persistent pain or stiffness post-surgery.
Long-Term Outlook (Prognosis)
Hip replacement offers excellent long-term results, with most patients experiencing 15–20 years of function from the prosthesis. Most individuals report significant pain relief and improved mobility after surgery, although high-impact activities like running are generally discouraged to preserve the longevity of the implant.
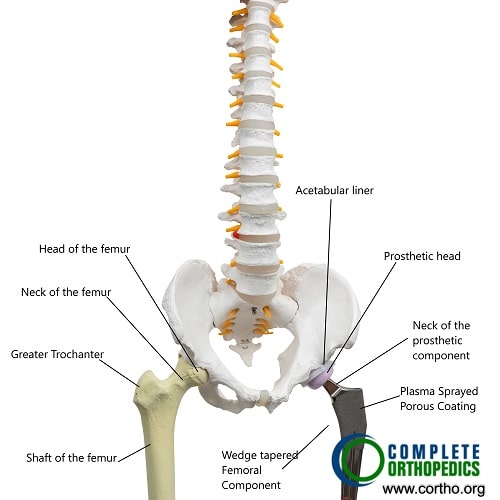
Total Hip Replacement
Out-of-Pocket Costs
Medicare
CPT Code 20902 – Bone Grafting (Harvest and Placement of Bone Graft): $63.66
CPT Code 27125 / 27130 – Hip Replacement (Partial / Total Hip Arthroplasty): $268.14 / $303.45
CPT Code 38220 – Bone Marrow Injection (Aspiration for Bone Marrow Concentrate Therapy): $36.05
Medicare Part B typically covers 80% of the approved cost for these procedures once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield usually cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries and procedures. These plans coordinate with Medicare to fill the coverage gap and reduce patient financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans typically cover any remaining balance, including coinsurance or small deductibles, which generally range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your avascular necrosis or hip injury requiring these procedures is work-related, Workers’ Compensation will cover all associated medical expenses, including surgery, bone grafting, and rehabilitation. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip condition or bone damage related to avascular necrosis is the result of an automobile accident, No-Fault Insurance will typically cover the total cost of treatment, including joint replacement, bone grafting, and bone marrow injections. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your policy.
Example
Jennifer Myers underwent bone grafting (CPT 20902) to treat avascular necrosis in her hip, followed by a total hip replacement (CPT 27130). Her estimated Medicare out-of-pocket cost was $63.66 for the bone graft and $303.45 for the total hip replacement. Since Jennifer had supplemental insurance through Blue Cross Blue Shield, her remaining balance was fully covered, leaving her with no out-of-pocket expenses for either procedure.
Frequently Asked Questions (FAQ)
Q. How long does a hip replacement last?
A. The artificial hip joint typically lasts 15–20 years, and some may last even longer with proper care.
Q. When can I return to work?
A. Sedentary jobs may allow you to return in 2–4 weeks, while more physically demanding jobs may require 6–12 weeks.
Q. Can I return to sports after surgery?
A. Low-impact activities like walking, swimming, and cycling are encouraged, but high-impact activities like running should be avoided.
Summary and Takeaway
Hip replacement is a proven, effective treatment for those suffering from chronic hip pain, especially when conservative treatments have failed. The procedure significantly improves pain relief and mobility, allowing patients to return to normal activities.
Clinical Insight & Recent Findings
A recent study explored the recovery journey of older adults after hip replacement surgery, highlighting the emotional, cognitive, and physical challenges they face. Participants experienced varying levels of pain, cognitive issues like memory loss, and emotional struggles such as fatigue.
However, staying active physically and socially helped many improve over time. By one year post-surgery, most reached a stable state, though recovery varied among individuals. (“Study on recovery experiences after hip replacement surgery – see PubMed.”)
Who Performs This Surgery? (Specialists and Team Involved)
Hip replacement surgery is performed by orthopedic surgeons specializing in joint replacements. The recovery team includes anesthesiologists, nurses, and physical therapists.
When to See a Specialist?
If you experience persistent hip pain, limited range of motion, or difficulty performing daily activities like walking, standing, or bending down, consult with an orthopedic surgeon.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience severe pain, signs of infection (fever, swelling, redness), or if you cannot move your hip post-surgery.
What Recovery Really Looks Like?
Recovery typically takes 6–12 weeks for basic activities and 6–12 months for full recovery. Early physical therapy and gradual return to activity are key components of a successful recovery.
What Happens If You Delay Surgery?
Delaying surgery can lead to increased pain, further joint deterioration, and limited mobility, making recovery after surgery more challenging. Early intervention provides the best outcomes.
How to Prevent Recurrence or Failure?
Maintaining strength and stability around the hip joint, avoiding high-impact activities, and following a structured rehabilitation program will help preserve the longevity of the hip replacement.
Nutrition and Bone or Joint Health
Eating a balanced diet rich in calcium, vitamin D, and lean proteins promotes bone health and aids recovery. Avoid smoking and excessive alcohol consumption for optimal recovery.
Activity and Lifestyle Modifications
Low-impact activities like walking, swimming, and cycling are recommended after surgery, while high-impact activities like running and heavy lifting should be avoided to ensure the longevity of the prosthesis.
Do you have more questions?
How can one prepare their home environment for post-surgery recovery?
Preparing the home may involve removing trip hazards, installing handrails or grab bars, and arranging for assistance with daily tasks if needed.
Can hip replacement surgery be performed on patients with other underlying health conditions?
Yes, but the patient’s overall health and the severity of their other conditions will be considered in determining surgical candidacy and planning.
Are there any specific precautions to prevent infection after surgery?
Precautions may include proper wound care, antibiotic prophylaxis, and avoiding environments where infection risk is high.
Can physical therapy be continued at home, and if so, how?
Yes, physical therapy exercises prescribed by a therapist can often be continued at home, with guidance on proper technique and progression.
What should one do if they experience unusual symptoms after hip replacement surgery?
It’s important to contact the surgeon or healthcare provider if experiencing unusual symptoms such as increased pain, swelling, or signs of infection.
How soon after surgery can one expect to resume normal daily activities?
Normal activities can usually be resumed gradually as tolerated, with guidance from the healthcare team.
Are there any restrictions on flying after hip replacement surgery?
It’s generally safe to fly after hip replacement surgery, but it’s recommended to wait at least 4 to 6 weeks and take precautions such as moving and stretching during the flight.
What is the typical length of hospital stay for hip replacement surgery?
Hospital stays typically range from 1 to 4 days, depending on individual recovery progress and surgical approach.
Are there any alternatives to hip replacement surgery?
Alternatives may include conservative treatments such as physical therapy, medications, injections, or other surgical procedures depending on the specific condition.
How often should the artificial hip joint be checked or monitored after surgery?
Regular follow-up appointments with the surgeon are typically scheduled to monitor the artificial joint’s function and detect any potential issues early.
Are there any specific exercises or activities to maintain hip health in the long term post-surgery?
Regular low-impact exercises such as walking, swimming, and cycling can help maintain hip health and overall mobility in the long term after surgery.
Are there any dietary restrictions to follow before or after surgery?
It’s important to maintain a healthy, balanced diet both before and after surgery to support healing and overall health. Specific dietary restrictions may vary based on individual medical conditions.
How long does the artificial hip joint typically last?
Artificial hip joints can last 15 to 20 years or more, depending on factors such as patient activity level and implant quality.
Are there any lifestyle changes recommended before or after hip replacement surgery?
Yes, lifestyle changes may include weight management, smoking cessation, and modifications to physical activities to reduce stress on the hip joint.
How long does a typical hip replacement surgery last?
The surgery typically lasts between 1 to 2 hours, depending on various factors such as the complexity of the case and surgical approach.
What are the different types of hip replacement surgeries available?
Different types include total hip replacement, partial hip replacement, and hip resurfacing.
How much does hip replacement surgery cost?
The cost varies depending on factors such as the surgical approach, equipment required, and implants used. Patients are advised to discuss cost breakdown with their orthopedic surgeon.
What exercises are typically recommended during hip replacement surgery recovery?
Strengthening exercises such as straight leg raises, clamshell raises, and wall squats are commonly included in the recovery regimen, tailored to the surgical approach used.
What is the typical recovery timeframe for hip replacement surgery?
Most patients achieve almost complete recovery within three months, with the majority of recovery occurring in the first six weeks, gradually regaining mobility and strength in the hip muscles.
What are the risks associated with hip replacement surgery?
Risks include heart attack, blood clots, stroke, infection, neurovascular injury, dislocation/instability, leg length discrepancy, and persistent postoperative pain, although strategies exist to minimize these risks.
What is the success rate of hip replacement surgery?
Hip replacement surgery has a success rate upwards of 95%, with the majority being around 97 to 98%, defined by improved pain, activity levels, and overall quality of life.
What is the procedure for hip replacement surgery?
The procedure involves gaining surgical access to the hip joint, removing the arthritic femoral head and socket, and replacing them with appropriately sized hip replacement implants to restore stability and leg length.
Who is considered a good candidate for hip replacement surgery?
Hip replacement surgery is usually reserved for elderly patients who have maximized benefits from nonsurgical management strategies, although it can be offered to younger patients who absolutely require it.
What strategies are typically tried before resorting to hip replacement surgery?
Non-surgical strategies may include using gait aids, taking analgesics such as nonsteroidal anti-inflammatory drugs or Tylenol, physical therapy, massage therapy, and injections.
What materials are used in hip replacement surgery?
The materials used include a femoral stem, an artificial femoral head, an acetabular component, bone screws, and an acetabular liner made of polyethylene.
What is osteoarthritis, and why is it the most common reason for hip replacement surgery?
Osteoarthritis is a condition that develops gradually over years, causing hip discomfort and pain that worsens over time, making it difficult for individuals to perform daily activities.
What are common symptoms experienced by individuals requiring hip replacement surgery?
Common symptoms include pain and discomfort in and around the hip joint, often felt in the groin, buttock area, or deep within the hip joint itself.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
