Back Pain
Back pain is one of the most common medical problems affecting people worldwide. Nearly 80% of adults experience back pain at some point in their lives. While most cases are temporary and improve with rest, exercise, and conservative treatment, severe or persistent back pain can interfere with daily life and may indicate an underlying spinal problem.
The good news is that most back pain can be managed successfully through proper diagnosis, physical therapy, medication, and—if needed—surgery.
How Common It Is and Who Gets It? (Epidemiology)
Back pain affects people of all ages but is most common between the ages of 30 and 60.
-
It is a leading cause of workplace absenteeism and disability.
-
Both men and women are equally affected.
-
The likelihood increases with age, poor posture, inactivity, and obesity.
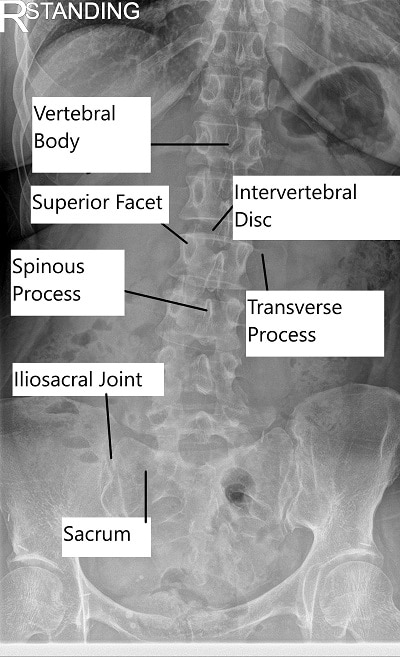
X-ray of the Lumbar Spine.
Why It Happens – Causes (Etiology and Pathophysiology)
Back pain can be mechanical, degenerative, or related to systemic disease. Common causes include:
-
Muscle or ligament strain: From lifting heavy objects, sudden movements, or poor posture.
-
Herniated or bulging discs: Discs act as cushions between vertebrae; when they rupture, they can press on nerves, causing pain or sciatica.
-
Arthritis and spinal stenosis: Wear-and-tear arthritis narrows the spinal canal, leading to nerve compression.
-
Osteoporosis: Weak, brittle bones can cause small compression fractures in the spine.
-
Infections or tumors: Rarely, spinal infections or cancer can cause pain.
-
Poor posture and inactivity: Weak core muscles and prolonged sitting contribute to mechanical pain.
Disclaimer – The above video content is external and shows the opinion of the involved vendor.
How the Body Part Normally Works? (Relevant Anatomy)
The spine is made up of 33 vertebrae stacked on top of one another, separated by soft intervertebral discs that act as shock absorbers. Muscles and ligaments around the spine provide stability and movement.
Pain occurs when these structures—bones, joints, discs, or muscles—are strained or compressed, irritating nearby nerves.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms of back pain include:
-
Dull, aching discomfort in the lower back.
-
Shooting or burning pain that travels down one leg (sciatica).
-
Muscle tightness or spasms.
-
Pain that worsens with activity but improves with rest.
-
Limited range of motion or stiffness when bending or twisting.
In severe cases, pain may radiate below the knee, or you may feel numbness, tingling, or weakness in one or both legs.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed history and physical exam to identify the cause of pain.
Imaging or lab tests may include:
-
X-rays: Reveal bone alignment or fractures.
-
MRI: Best for detecting disc herniation, nerve compression, or soft tissue issues.
-
CT scan: Provides detailed bone images.
-
Blood tests: Help detect infection, inflammation, or systemic diseases.
In rare cases, additional studies like bone scans or nerve conduction tests (EMG/NCS) may be ordered.
Classification
Back pain is classified by duration and underlying cause:
-
Acute: Lasts less than 6 weeks.
-
Subacute: Lasts 6–12 weeks.
-
Chronic: Persists beyond 3 months.
It can also be divided into mechanical (structural) and non-mechanical (systemic or referred) pain.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Kidney stones or infections
-
Aortic aneurysm
-
Pelvic or ovarian disease
-
Hip or sacroiliac joint dysfunction
-
Spinal tumors or infections
Treatment Options
Non-Surgical Care
Most cases of back pain improve with conservative care:
-
Medications:
-
Over-the-counter pain relievers (acetaminophen, NSAIDs).
-
Prescription muscle relaxants or nerve pain medications if needed.
-
-
Physical therapy: Strengthens core muscles, improves flexibility, and corrects posture.
-
Heat and cold therapy: Reduces inflammation and soothes sore muscles.
-
Lifestyle changes: Maintain a healthy weight, avoid smoking, and stay physically active.
-
Alternative therapies: Acupuncture, chiropractic care, or massage may provide additional relief.
-
Injections: Epidural steroid or facet injections may reduce inflammation and pain.
Surgical Care
Surgery is reserved for patients with persistent or severe pain due to structural issues such as herniated discs, spinal stenosis, or instability.
Common procedures include:
-
Discectomy: Removes the herniated portion of a disc.
-
Laminectomy: Removes part of a vertebra to relieve pressure on nerves.
-
Spinal fusion: Stabilizes the spine using screws and rods to join two or more vertebrae.
Recovery and What to Expect After Treatment
-
Conservative treatment: Most patients recover within 4–6 weeks.
-
After surgery: Recovery takes 1–4 months, depending on the procedure.
Physical therapy and gradual return to activity are vital for long-term success.
Possible Risks or Side Effects (Complications)
-
Persistent or recurring pain
-
Nerve injury or infection after surgery
-
Muscle weakness from inactivity
-
Complications from medication (stomach upset, drowsiness)
Long-Term Outlook (Prognosis)
Most people fully recover from back pain and return to normal activities. However, recurrence is common, especially if posture, core strength, and body mechanics are not maintained. Chronic back pain may require ongoing management and lifestyle changes.
Out-of-Pocket Costs
Medicare
CPT Code 63047 – Laminectomy (Decompression): $271.76
CPT Code 63030 – Discectomy (Removal of Herniated Disc): $225.06
CPT Code 22612 – Fusion (Posterior Lumbar Fusion): $382.85
CPT Code 22842 – Instrumentation (Rods, Screws, Plates – 3–6 Segments): $185.26
CPT Code 22867 – Interspinous Process Device Placement: $257.99
Under Medicare, 80% of the approved amount for these procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—are designed to cover this 20%, ensuring that most patients have little to no out-of-pocket expenses for Medicare-approved surgeries. These supplemental plans work directly with Medicare to provide complete coverage for decompression, fusion, instrumentation, and interspinous stabilization procedures.
If you have secondary insurance—such as Employer-Based Plans, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare has processed your claim. After the deductible is satisfied, these plans can cover any remaining coinsurance or balance. Most secondary insurance plans have small deductibles, typically between $100 and $300, depending on your policy and network of care providers.
Workers’ Compensation
If your lumbar spine condition or injury requiring decompression, fusion, or interspinous device placement was caused by work-related activities, Workers’ Compensation will pay for all related hospital, surgical, and rehabilitation costs. Patients will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your spinal condition or injury occurred or worsened due to a motor vehicle accident, No-Fault Insurance will cover the entire cost of treatment, including laminectomy, discectomy, fusion, and interspinous device placement. The only potential cost to you may be a small deductible depending on your insurance policy’s terms.
Example
Robert, a 68-year-old patient with lumbar spinal stenosis, underwent laminectomy (CPT 63047), posterior fusion (CPT 22612), and interspinous device placement (CPT 22867). His Medicare out-of-pocket costs were $271.76, $382.85, and $257.99. Because he had supplemental insurance through Blue Cross Blue Shield, the remaining 20% not covered by Medicare was fully paid, leaving him with no out-of-pocket expenses for his procedure.
Frequently Asked Questions (FAQ)
Q. What is the most common cause of back pain?
A. The majority of back pain cases are due to mechanical causes, such as muscle strain, disc problems, or arthritis, rather than serious illness.
Q. When should I see a doctor for back pain?
A. If pain lasts more than two weeks, radiates to the legs, or is accompanied by weakness, numbness, or bladder/bowel changes, seek medical evaluation.
Q. Can back pain be prevented?
A. Yes. Regular exercise, maintaining good posture, and using proper lifting techniques are key preventive measures.
Q. Do I always need surgery for back pain?
A. No. Over 90% of patients improve with non-surgical treatments such as physical therapy and medications. Surgery is only recommended for persistent or severe nerve compression.
Summary and Takeaway
Back pain is an extremely common but often manageable condition. Most cases resolve with conservative treatment, including rest, exercise, and medication. For severe cases caused by nerve compression or spinal instability, modern surgical techniques provide excellent results and rapid recovery. Maintaining a healthy lifestyle and proper posture can help prevent recurrence.
Clinical Insight & Recent Findings
A recent review highlighted that back pain remains one of the most common causes of disability worldwide, accounting for up to $200 billion annually in healthcare costs and lost productivity. The study classified causes into mechanical (90% of cases), inflammatory, infectious, oncologic, and metabolic origins, emphasizing that identifying red flags such as fever, trauma, cancer history, or neurological deficits is essential to avoid missing serious conditions like cauda equina syndrome or malignancy.
Evidence showed that most nonspecific back pain resolves with conservative management focusing on physical activity, education, and lifestyle modification rather than imaging or early pharmacologic intervention. First-line treatments include reassurance, early mobilization, and physical therapy, while NSAIDs or muscle relaxants may be used as adjuncts.
Surgery is reserved for persistent pain with neurological compromise or structural abnormalities. The review concluded that interprofessional management—combining physician guidance, physiotherapy, pharmacological care, and patient education—significantly improves recovery and reduces recurrence. (Study of multidisciplinary management and conservative care strategies for back pain – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Back pain is managed by a multidisciplinary team including orthopedic spine surgeons, neurosurgeons, pain management specialists, and physical therapists.
When to See a Specialist?
See a spine specialist if you experience:
-
Persistent back pain lasting more than 6 weeks.
-
Radiating pain, numbness, or tingling in the legs.
-
Difficulty walking or standing.
-
Pain following trauma or injury.
When to Go to the Emergency Room?
Seek immediate medical care if you experience:
-
Loss of bladder or bowel control.
-
Severe weakness or paralysis in the legs.
-
Fever, chills, or unexplained weight loss.
-
Pain after a serious fall or accident.
What Recovery Really Looks Like?
Most patients improve significantly within weeks through therapy and lifestyle adjustments. After surgery, gradual rehabilitation helps restore strength and flexibility. Ongoing exercise and good ergonomics prevent recurrence.
What Happens If You Ignore It?
Ignoring back pain can lead to chronic pain, nerve compression, or long-term mobility problems. Early diagnosis and treatment ensure faster recovery and prevent complications.
How to Prevent It?
-
Exercise regularly to strengthen core muscles.
-
Maintain proper posture when sitting and standing.
-
Lift objects correctly by bending at the knees.
-
Maintain a healthy weight and avoid smoking.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and lean protein supports bone and joint strength. Staying hydrated helps keep spinal discs healthy.
Activity and Lifestyle Modifications
Incorporate low-impact exercises such as walking, swimming, or yoga into your routine. Avoid prolonged sitting, use ergonomic chairs, and take frequent breaks during work.
Do you have more questions?
When should I consider seeing a doctor for my back pain?
You should see a doctor if you experience severe pain, pain that doesn’t improve with rest, or if it’s accompanied by symptoms like numbness, tingling, weakness, or bowel/bladder issues.
How does poor posture contribute to back pain?
Poor posture can strain muscles and ligaments, leading to discomfort and chronic back pain over time. It can also contribute to spinal misalignment.
What lifestyle changes can help prevent back pain?
Maintaining a healthy weight, regular exercise, good posture, and ergonomic adjustments at work can help prevent back pain.
What are the symptoms of a herniated disc?
Symptoms include localized back pain, pain radiating to the legs (sciatica), numbness, tingling, and weakness in the legs.
What is lumbar radiculopathy?
Lumbar radiculopathy, or sciatica, occurs when a nerve in the lower spine is compressed, causing pain, numbness, or weakness in the legs.
Can stress and anxiety cause back pain?
Yes, stress and anxiety can cause muscle tension and exacerbate back pain.
What are the surgical options for treating back pain?
Surgical options include microdiscectomy, spinal fusion, and decompression surgeries, depending on the underlying cause
How effective is physical therapy for back pain?
Physical therapy can be very effective for strengthening back muscles, improving flexibility, and reducing pain.
What role does obesity play in back pain?
Obesity increases the strain on the spine and back muscles, contributing to pain and the development of conditions like herniated discs.
How does smoking affect back pain?
Smoking can reduce blood flow to the spine, impairing healing and increasing the risk of back pain.
What are the risks of prolonged corticosteroid use for back pain?
Risks include weakened bones (osteoporosis), increased risk of infections, and potential hormonal imbalances.
What is osteoporosis and how does it relate to back pain?
Osteoporosis is a condition where bones become weak and brittle, often leading to fractures and chronic back pain.
Are there specific exercises recommended for back pain relief?
Yes, exercises like stretching, strengthening the core, and low-impact aerobic activities are recommended for back pain relief.
How does pregnancy contribute to back pain?
Pregnancy increases weight and changes posture, leading to additional strain on the back muscles and spine.
What are the benefits of using heat or ice for back pain?
Ice can reduce inflammation and numb acute pain, while heat can relax muscles and improve blood flow for chronic pain.
Can poor sleeping habits cause back pain?
Yes, improper sleeping positions or using a non-supportive mattress can contribute to back pain.
What is the significance of “red flags” in back pain assessment?
Red flags indicate serious conditions that require immediate medical attention, such as cancer, infections, or significant neurological deficits.
How does physical work affect back pain risk?
Arduous physical work can strain the back muscles and spine, increasing the risk of injury and chronic pain.
Can back pain be a symptom of other underlying health conditions?
Yes, back pain can be associated with conditions like kidney problems, infections, or tumors.
What is microdiscectomy and when is it used?
Microdiscectomy is a minimally invasive surgery to remove part of a herniated disc that is compressing a nerve, used when conservative treatments fail.
How long does recovery from back surgery typically take?
Recovery can take from 1 to 4 months or more, depending on the type of surgery and individual patient factors.
What role does ergonomics play in preventing back pain?
Proper ergonomics in the workplace and daily activities can help reduce strain on the back and prevent pain.
What is spinal fusion surgery and when is it recommended?
Spinal fusion surgery involves joining two or more vertebrae to stabilize the spine, recommended for conditions like severe degenerative disc disease or spondylolisthesis.
What are the potential complications of back surgery?
Complications can include infection, nerve damage, blood clots, and incomplete pain relief.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
