Total Hip Joint Dislocation
Hip replacement surgery provides relief from chronic hip pain caused by arthritis and other diseases. Patients return to the activities they enjoy benefiting from increased mobility.
Although total Hip replacement remains one of the most successful surgeries in modern medicine, not all patients have perfect outcomes.
One of the dreaded complications of hip replacement surgery is dislocation. Hip dislocation is uncommon but may occur in about 2% of patients, mostly within the first year of the surgery. Dislocation rates are significantly higher in revision surgeries.
A dislocation after hip replacement occurs when the ball of the prosthetic implant is displaced from the socket, causing severe discomfort and potential instability. Dislocation can happen due to various factors, including surgical approach, patient characteristics, and implant positioning. While total hip replacement is a highly successful surgery for treating hip arthritis, it requires careful planning to prevent complications like dislocation.
How Common It Is and Who Gets It? (Epidemiology)
Dislocation following total hip replacement is a rare complication, but it remains a concern, particularly in the first few months after surgery. The risk of dislocation is higher in patients undergoing the posterior approach (from behind the hip), older adults, and those with conditions that affect balance or neuromuscular control. Individuals who are non-compliant with post-operative precautions or have poor alignment of the hip prosthesis are also at an increased risk.
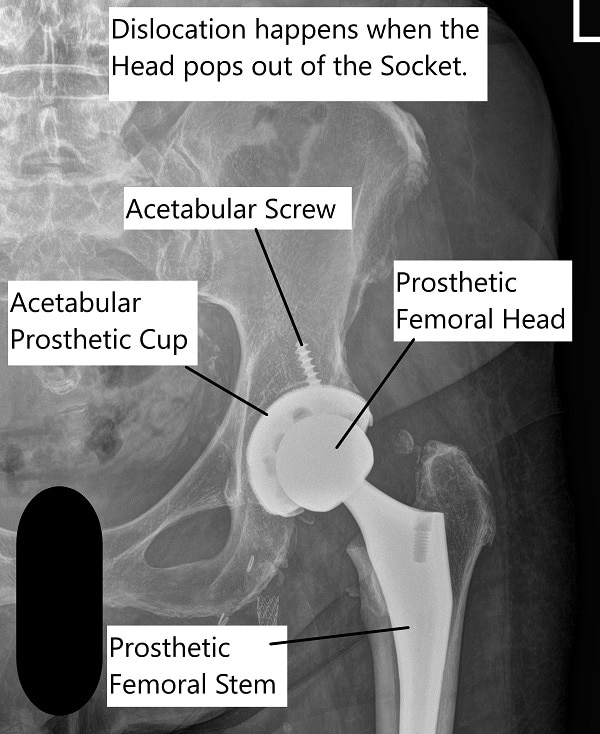
Total Hip Arthroplasty dislocation
Why It Happens – Causes (Etiology and Pathophysiology)
Dislocation occurs when the femoral head (the ball part of the implant) is pushed out of the acetabulum (the socket). Factors contributing to dislocation include:
-
Surgical approach: The posterior approach is more prone to dislocation, while the anterior approach is less invasive.
-
Implant positioning: Incorrect placement of the implant can increase the risk of dislocation.
-
Patient factors: Age, obesity, neuromuscular conditions, prior surgeries, and developmental hip disorders such as hip dysplasia can contribute to hip instability.
-
Post-surgical factors: Not adhering to hip precautions after surgery, such as avoiding movements that place the hip in a vulnerable position (e.g., bending the hip beyond 90 degrees), increases the risk of dislocation.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint where the femoral head fits into the acetabulum. The joint is stabilized by ligaments, muscles, and a joint capsule. After total hip replacement, the prosthetic ball (femoral head) and socket (acetabular cup) are designed to mimic the natural anatomy. The alignment and positioning of these components are crucial for preventing dislocation and ensuring smooth, pain-free movement.
What You Might Feel – Symptoms (Clinical Presentation)
When a dislocation occurs, patients often experience sudden and severe pain, an inability to move the hip joint, and difficulty bearing weight on the affected side. The leg may appear twisted or out of alignment. Dislocations often happen quickly, and patients may feel an immediate, intense pain and be unable to move the joint without assistance.
How Doctors Find the Problem? (Diagnosis and Imaging)
A dislocation is diagnosed through physical examination, where the doctor checks for signs of hip misalignment. X-rays or CT scans are used to confirm the dislocation and assess the positioning of the implant components. Imaging also helps to rule out other complications, such as fractures or implant loosening.
Classification
Dislocation after hip replacement can be classified based on the direction of the dislocation:
-
Anterior dislocation: Occurs when the femoral head moves forward, more common in anterior approach surgeries.
-
Posterior dislocation: Occurs when the femoral head moves backward, more common in posterior approach surgeries.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic dislocation include implant loosening, hip fractures, nerve impingement, or infection. Patients experiencing severe pain, limited mobility, or abnormal positioning should seek immediate evaluation to rule out these conditions.
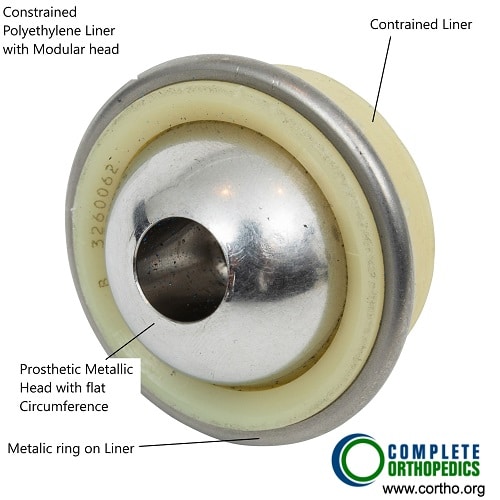
Constrained Liner
Treatment Options
Non-Surgical Care – If the dislocation is diagnosed early, the femoral head can be repositioned into the socket through a process called hip reduction. This procedure is typically performed under sedation or anesthesia. After reduction, the patient may be placed in a brace to stabilize the joint and prevent further dislocation.
Surgical Care – If the dislocation recurs or is caused by incorrect implant alignment, revision surgery may be necessary. This surgery repositions the implant components or uses specialized implants to prevent future dislocations.
-
Dual mobility head and liner: This design allows the femoral head to move more freely within the acetabulum while maintaining stability, reducing the risk of dislocation.
-
Acetabular liner with elevated lip: This liner design deepens the socket, making it harder for the femoral head to dislocate.
-
Robotic-assisted surgery: Robotic systems help ensure precise implant placement, reducing the risk of dislocation.
Recovery and What to Expect After Treatment
Most patients who undergo hip reduction can return home the same day, but they will need to follow hip precautions to ensure proper healing and prevent further dislocations. After surgical correction, recovery may take several weeks, with physical therapy playing an essential role in restoring strength, stability, and range of motion. Full recovery may take months, depending on the type of procedure performed.
Possible Risks or Side Effects (Complications)
Potential complications following a dislocation include nerve damage, infection, blood clots, further dislocations, and joint stiffness. Revision surgeries carry additional risks, including longer recovery times and more complex rehabilitation.
Long-Term Outlook (Prognosis)
The prognosis for hip replacement dislocation is generally good with proper treatment. Most patients recover without further incidents, especially if they adhere to post-operative precautions and follow-up care. In cases requiring revision surgery, outcomes are usually favorable, but recovery can take longer.
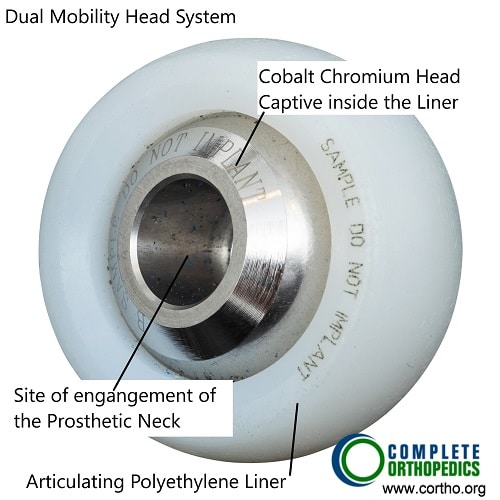
Dual mobility head and liner
Out-of-Pocket Costs
Medicare
CPT Code 27265 – Closed Reduction (No Anesthesia) for Post-THA Dislocation: $101.48
CPT Code 27266 – Closed Reduction (With Anesthesia) for Post-THA Dislocation: $139.15
CPT Code 27268 – Open Reduction for Post-THA Dislocation: $131.12
CPT Code 27134 – Revision of Both Components (Total Hip Replacement, Acetabular and Femoral Components): $448.00
CPT Code 27137 – Revision of Acetabular Component Only: $345.69
CPT Code 27138 – Revision of Femoral Component Only: $359.01
Medicare Part B typically covers 80% of the approved cost for these procedures after your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans work alongside Medicare to fill the coverage gap and reduce financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which typically range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your hip dislocation or revision hip replacement surgery is required due to a work-related injury, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly pays for all approved treatments.
No-Fault Insurance
If your hip dislocation or revision surgery is the result of an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including closed or open reduction and subsequent revision surgeries. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
John Foster experienced a post-THA dislocation and required closed reduction with anesthesia (CPT 27266), with an estimated Medicare out-of-pocket cost of $139.15. Later, he required a revision of both components (CPT 27134) due to complications, with an estimated cost of $448.00. Since John had supplemental insurance through Blue Cross Blue Shield, both amounts were fully covered, leaving him with no out-of-pocket expenses for the procedures.
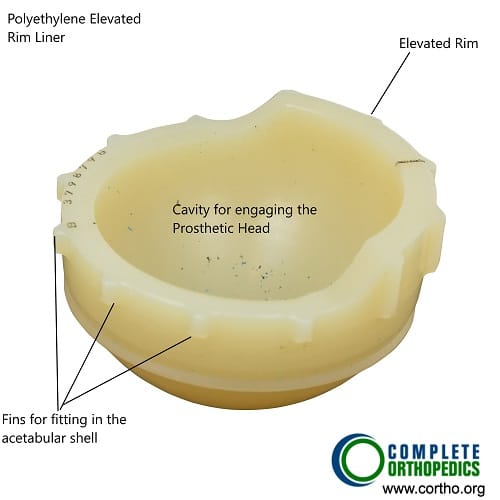
Acetabular liner with elevated lip
Frequently Asked Questions (FAQ)
Q. Is hip dislocation after surgery common?
A. No, it’s a rare complication. However, it is more likely during the first few months post-surgery, especially if hip precautions are not followed.
Q. What can I do to avoid dislocation?
A. Follow your surgeon’s instructions carefully, especially the hip precautions, and avoid movements that could place stress on the joint.
Q. How long does it take to recover from a hip dislocation?
A. Most people recover within a few weeks after the hip reduction, though surgery for recurrent dislocations may require a few months for full recovery.
Summary and Takeaway
Dislocation after total hip replacement is rare but can cause significant pain and complications. Early intervention, including hip reduction or revision surgery, is typically effective. Following hip precautions and working with your healthcare team can significantly reduce the risk of dislocation and help ensure a successful recovery.
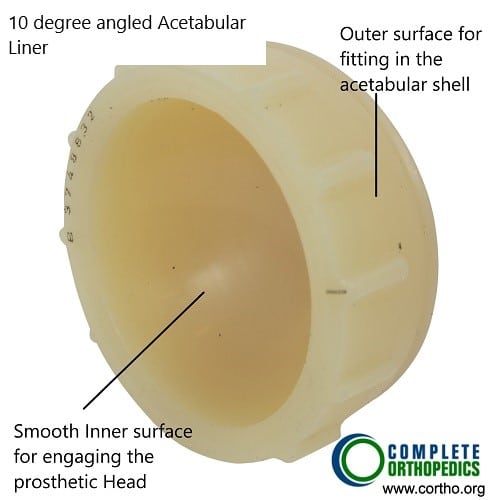
10 Degree angled acetabular liner
Do you have more questions?
What are the risk factors for total hip joint dislocation?
Risk factors for total hip joint dislocation include advanced age, previous hip surgeries, congenital hip abnormalities, and certain medical conditions affecting joint stability.
Can total hip joint dislocation occur spontaneously, without any traumatic event?
While uncommon, total hip joint dislocation can occur spontaneously in individuals with certain predisposing factors such as ligamentous laxity or muscle weakness.
What are the symptoms of total hip joint dislocation?
Symptoms of total hip joint dislocation include severe pain, inability to bear weight on the affected leg, visible deformity or abnormal positioning of the hip, and limited range of motion.
Is total hip joint dislocation a medical emergency?
Yes, total hip joint dislocation is considered a medical emergency that requires immediate evaluation and treatment to prevent complications such as nerve or blood vessel injury.
What complications can arise from total hip joint dislocation?
Complications of total hip joint dislocation may include nerve damage, vascular injury, fracture of the hip socket or femur, avascular necrosis of the femoral head, and long-term joint instability.
What is the typical treatment approach for total hip joint dislocation?
The treatment of total hip joint dislocation often involves closed reduction, where the hip joint is manually manipulated back into its normal position under anesthesia. In some cases, surgical intervention may be necessary to stabilize the joint.
How successful is closed reduction in treating total hip joint dislocation?
Closed reduction is often successful in restoring normal hip joint alignment and function, especially when performed promptly after the dislocation occurs. However, the success rate may vary depending on factors such as the severity of the dislocation and associated injuries.
Can total hip joint dislocation lead to chronic hip instability or recurrent dislocations?
Yes, untreated or inadequately managed total hip joint dislocation can lead to chronic hip instability or recurrent dislocations, especially in cases where there is underlying ligamentous laxity or structural abnormalities.
What is the role of physical therapy in the rehabilitation of total hip joint dislocation?
Physical therapy plays a crucial role in the rehabilitation of total hip joint dislocation by restoring strength, range of motion, and stability to the hip joint, as well as addressing any residual muscle weakness or imbalances.
Are there any restrictions or precautions that should be followed after experiencing a total hip joint dislocation?
Yes, individuals who have experienced a total hip joint dislocation may be advised to avoid certain activities or movements that could place excessive stress on the hip joint, such as high-impact sports or activities that involve extreme ranges of motion.
How long does it take to recover from a total hip joint dislocation, and what is the expected timeline for return to normal activities?
The recovery time for a total hip joint dislocation depends on factors such as the severity of the dislocation, associated injuries, and the individual’s overall health. Rehabilitation and return to normal activities may take several weeks to months.
Can total hip joint dislocation lead to long-term complications such as hip arthritis?
Yes, total hip joint dislocation can increase the risk of long-term complications such as hip arthritis due to damage to the cartilage and supporting structures of the joint.
How does the age of the individual impact the treatment and prognosis of total hip joint dislocation?
The age of the individual can influence the treatment approach and prognosis of total hip joint dislocation, with younger patients often having a better chance of full recovery and lower risk of long-term complications.
Can total hip joint dislocation affect mobility and independence in daily activities?
Yes, total hip joint dislocation can significantly affect mobility and independence in daily activities, particularly if there are associated injuries or complications that limit hip function.
Are there any measures that can be taken to prevent total hip joint dislocation in individuals at risk, such as those with hip dysplasia?
Individuals at risk of total hip joint dislocation, such as those with hip dysplasia, may benefit from lifestyle modifications, physical therapy, and orthopedic interventions aimed at improving hip stability and preventing traumatic injuries.
How does the presence of other medical conditions, such as osteoporosis or rheumatoid arthritis, affect the management of total hip joint dislocation?
Other medical conditions such as osteoporosis or rheumatoid arthritis may complicate the management of total hip joint dislocation by increasing the risk of fracture or affecting bone healing. Close coordination with other specialists may be necessary for comprehensive care.
Can total hip joint dislocation cause damage to surrounding structures such as nerves or blood vessels?
Yes, total hip joint dislocation can cause damage to surrounding structures such as nerves or blood vessels, especially if the dislocation is severe or if there are associated fractures.
How does the mechanism of injury influence the severity and treatment of total hip joint dislocation?
The mechanism of injury, such as the direction and force of impact, can influence the severity and treatment of total hip joint dislocation. For example, high-energy traumas may result in more extensive soft tissue damage and require surgical intervention for stabilization.
Can total hip joint dislocation affect other joints or areas of the body, such as the lower back or knees?
Yes, total hip joint dislocation can affect other joints or areas of the body indirectly through compensatory movements or altered biomechanics, potentially leading to secondary pain or dysfunction. Rehabilitation and addressing underlying issues are important for overall recovery and function.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
