Total Hip Replacement Implants
Total hip replacement (THR) is a widely successful surgery designed to alleviate pain and improve mobility for patients suffering from hip arthritis, fractures, or other degenerative joint conditions. During the procedure, the damaged femoral head and acetabulum (hip socket) are replaced with prosthetic components. The materials and design of the implants are crucial factors in the surgery’s success, as the right prosthetic components ensure proper function, durability, and a reduction in wear and tear over time. This article explores the different hip replacement implant designs, their materials, and the factors that influence their use in surgery.
Functional Anatomy
The hip joint is a ball-and-socket joint composed of the femoral head (ball) and the acetabulum (socket) in the pelvis. The femoral head fits into the acetabulum, enabling the smooth, multi-directional movement of the leg. The joint is stabilized by ligaments, muscles, and articular cartilage. In hip replacement surgery, the femoral head and acetabulum are replaced by artificial components that mimic the natural motion of the joint. The choice of implant material and design plays a critical role in the long-term durability and functionality of the prosthesis.
Biomechanics or Physiology
The success of total hip replacement depends on how well the prosthetic components replicate the natural biomechanics of the hip joint. The prosthetic femoral head and acetabular component must fit properly and align with the natural angles of the femoral neck to ensure stability and smooth movement. The bearing surface between the femoral head and acetabulum must allow for frictionless motion while being durable enough to withstand repetitive use. Materials like polyethylene, ceramic, and metal are chosen based on their ability to handle the forces involved in daily activities, such as walking, standing, and climbing stairs.
Common Variants and Anomalies
Total hip replacements can vary in the type of prosthetic components used, as well as the material of the bearing surface:
-
Hard-on-soft bearing: This design includes a metal ball paired with a polyethylene socket liner. Polyethylene is highly cross-linked to improve durability and reduce wear.
-
Hard-on-hard bearing: This includes a metal ball paired with a metal cup or a ceramic ball with a ceramic cup. This design minimizes wear and tear but may be associated with higher friction and noise (e.g., squeaking) in some cases.
-
Ceramic-on-ceramic: Ceramic implants are smoother, scratch-resistant, and more durable, reducing wear particles over time. However, they are more fragile and sensitive to implant positioning.
The choice of implant design and materials depends on the patient’s age, activity level, and bone quality.
Implants
An ideal implant should last duplicate the function of the natural joint. The artificial hip should allow natural movements for the patients to do the activities they enjoy. The implant should be non-allergic and have a good track record. The implant should have a low degree of friction and less generation of wear and tear particles.
An ideal implant should last a patient’s lifespan. Most implants last on an average for 15-20 years or more. The choice of implant used also depends upon the surgeon’s familiarity with the implant and expertise. Currently used implants may either be hard-on-soft bearing or hard-on-hard bearings.
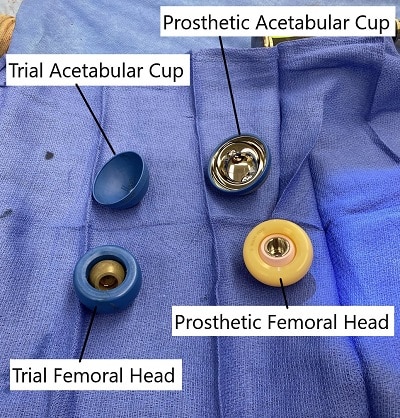
Trial and Actual Implant (Head of femur and Acetabular Component)
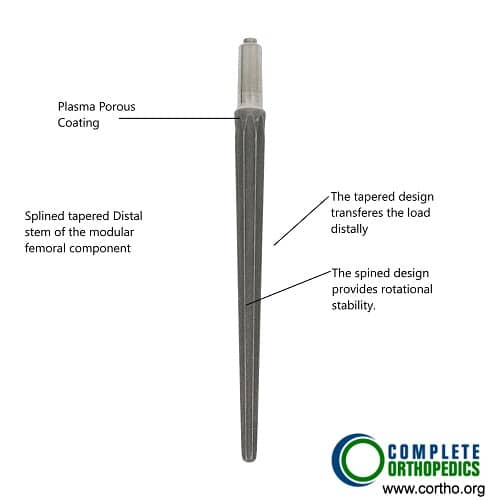
Splined modular distal femoral component
The image shows a splined tapered modular distal femoral prosthetic component. The tapered end allows ease of insertion and the splined design provides rotational stability in the femoral canal. The modular implants are commonly used in revision hip replacement surgery. The special design allows to achieve greater stability in the event of encountering bone loss during extraction.
Hard-on-soft bearing
The ball is made of metal and the cup is made of specialized plastic called polyethylene. The polyethylene plastic is highly cross-linked to make it resistant to wear and tear. The metal may be made of a cobalt-chromium alloy or ceramic. The metal ball and a polyethylene liner is currently the most commonly used bearing surface.
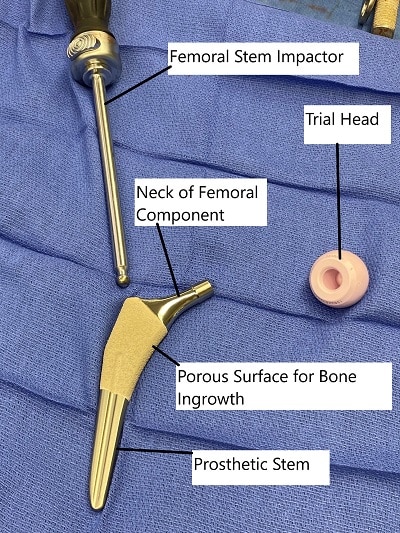
Total Hip Replacement Components.
Ceramic is a harder surface than the cobalt-chromium alloy. The ceramic surface is ultra-smooth and scratch-resistant. Due to these properties, ceramic has extremely low generation of wear and tear particles.
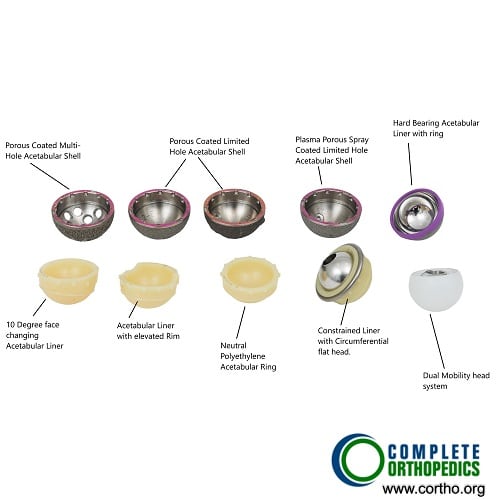
Different types of acetabular liners and shells
There are different types of acetabular liners and shells. Neutral liners are commonly used in primary surgeries. Lateralized liners and acetabular liners with elevated rims may be used in revision surgeries to prevent dislocation. Constrained liners and dual mobility heads are used in cases of total hip replacement dislocation.
Hard-hard bearing
These bearing surfaces can either be a metal ball on a metal cup or ceramic ball on a ceramic cup. The surface of the metal/ceramic implants may be made rough to allow the bone to grow on the implant. The metal alloy may be highly carbonized to decrease the generation of wear and tear particles.
The advantage of hard-on-hard bearing surfaces is reduced chances of dislocation. The hard-on-hard bearing surfaces are able to accommodate a large size of the ball (femoral head). A larger size of the ball reduces the chance of dislocation.

Hard bearing acetabular liner
The hard bearing acetabular liner comes with an inserter ring to prevent micromotion. The large cavity of the metallic liner allows insertion of a large prosthetic head of femur therefore limiting the chances of dislocation.
A disadvantage of hard-on-hard metal alloy implants is the generation of wear and tear particles. The levels of the alloy (cobalt-chromium) may be increased in the blood. These implants are therefore avoided in patients with kidney failure. The implants are also avoided in patients of childbearing age group.
The metal alloy wear particles may cause aseptic vasculitis associated vascular lesion (ALVAL). The immune cells of the body may accumulate around the implant and cause erosion of the bone and inflammation of the tissues. These may also cause the formation of a solid mass known as a pseudotumor.
The ceramic hips are generally made of alumina ceramic. The alumina ceramic has a very high density and therefore has an extremely smooth surface. The smooth surface allows decreased friction. The implants are also hydrophilic (water retaining), that allows a small film of water on the surface leading to lubrication.
The ceramic implants are also scratch-resistant and are inert in the body. The ceramic implants are extremely sensitive to implant position. Malpositioned ceramic implants may lead to failure. Ceramic implants may also press against each other at the outer boundary to cause chip fracture. The implants may also produce a squeaking sound.
Clinical Relevance
Total hip replacement surgery is often recommended for patients with severe hip pain and restricted mobility due to arthritis or femoral fractures. The prosthetic components used in THR must replicate the joint’s natural function and allow for smooth movement, while providing durability for long-term use. Choosing the right implant materials (metal, ceramic, or polyethylene) and fixation method (cemented or uncemented) is critical for the success of the surgery. Surgeons consider patient factors such as activity level and bone quality when selecting the appropriate implant.
Imaging Overview
-
X-rays are the first-line imaging modality for evaluating the alignment, fit, and placement of the prosthetic components post-surgery.
-
CT scans may be used to assess bone quality around the implant, especially if there are concerns about implant loosening or wear.
-
MRI is not typically used for the hip joint due to the presence of metal implants, but it can help assess soft tissue damage in patients with complications such as infection or impingement.
-
Bone scans are sometimes used to monitor implant performance, looking for early signs of implant loosening or osteolysis (bone resorption).
Associated Conditions
Patients requiring hip replacement surgery often suffer from the following conditions:
-
Osteoarthritis: The leading cause of hip replacement, characterized by the breakdown of joint cartilage.
-
Rheumatoid arthritis: An autoimmune disease that causes inflammation and degeneration of joint tissue.
-
Osteonecrosis: Loss of blood supply to the femoral head, resulting in bone death and collapse.
-
Hip fractures: Severe fractures from trauma that compromise the hip joint’s function.
-
Developmental hip issues: Conditions like hip dysplasia or Legg-Calvé-Perthes disease that affect the hip joint early in life but may lead to arthritis later.
Surgical or Diagnostic Applications
Total hip replacement surgery is performed when conservative treatments such as pain medications, physical therapy, and assistive devices fail to alleviate symptoms. The procedure involves:
-
Incision: The surgeon makes an incision over the hip, which can be done via posterior, anterior, or lateral approaches.
-
Removal of damaged bone and cartilage: The femoral head and acetabulum are removed, and prosthetic components are inserted.
-
Fixation: Components are press-fit into the bone or secured using bone cement.
-
Positioning: The components are aligned to restore the natural angles of the hip joint to ensure proper stability and function.
Prevention and Maintenance
To maintain a long-lasting hip replacement and avoid complications:
-
Maintain a healthy weight to reduce stress on the implant.
-
Avoid high-impact activities such as running or jumping to prevent premature wear.
-
Follow a rehabilitation plan that includes strengthening exercises to restore muscle function and prevent instability.
-
Monitor for signs of complications, such as dislocation, loosening, or infection, with regular follow-up care and imaging.
Research Spotlight
A recent study highlighted the growing importance of advanced porous hip implants in reducing complications commonly associated with traditional solid implants, such as stress shielding and cortical hypertrophy. Porous implants, fabricated using additive manufacturing, can more closely mimic the natural structure of bone, promoting better osseointegration and reducing the likelihood of implant failure. These implants offer improved mechanical properties, such as a lower elastic modulus and higher energy absorption, which better align with the surrounding bone tissue. The study emphasized that the optimization of porous structures, including lattice designs and triply periodic minimal surfaces (TPMS), significantly enhances the stress distribution on the femur, reducing bone resorption and improving long-term stability. These findings suggest that incorporating porous structures in hip implants can lead to better outcomes, especially in patients with lower bone quality, by minimizing stress shielding and promoting more effective bone healing. (“Study on porous implants in hip replacement – See PubMed.”)
Summary and Key Takeaways
-
Total hip replacement surgery is highly effective in relieving pain and improving mobility for patients with hip arthritis or joint degeneration.
-
Postoperative rehabilitation and physical therapy are essential for restoring strength, range of motion, and functional recovery.
-
Implant materials and surgical approaches are tailored to the patient’s age, activity level, and bone quality.
-
Robot-assisted surgery and ceramic-on-ceramic implants show promising results in improving accuracy and reducing wear, especially for younger patients.
-
Long-term success depends on regular follow-up, activity modifications, and prevention of high-impact stress on the joint.
References / Citations (Optional)
American Academy of Orthopaedic Surgeons. “Total Hip Replacement.”
Do you have more questions?
Are there different designs of total hip replacement implants available, and how do they vary in terms of stability and longevity?
Yes, there are various designs of total hip replacement implants, including cemented, uncemented, and hybrid designs, each with its advantages and considerations regarding stability and longevity.
Can total hip replacement implants be customized to fit a patient’s specific anatomy, or are they standardized?
Total hip replacement implants can be customized to some extent to fit a patient’s specific anatomy, with options for different sizes, shapes, and configurations to optimize fit and function.
What are the potential complications associated with total hip replacement implants, such as loosening or wear of the implant components?
Potential complications of total hip replacement implants include implant loosening, wear of the implant components, dislocation, infection, nerve or blood vessel injury, and allergic reactions to implant materials.
How long do total hip replacement implants typically last, and what factors influence their longevity?
The longevity of total hip replacement implants varies depending on factors such as patient age, activity level, implant type, surgical technique, and the presence of any complications or underlying conditions.
Can total hip replacement implants be revised or replaced if they wear out or fail over time?
Yes, total hip replacement implants can be revised or replaced through a surgical procedure known as revision hip replacement if they wear out or fail over time. This involves removing the old implants and replacing them with new ones.
Are there any restrictions on physical activities or movements for individuals with total hip replacement implants?
While total hip replacement implants can significantly improve mobility and function, some restrictions on high-impact activities or extreme ranges of motion may be advised to minimize the risk of implant wear or dislocation.
How does the surgical approach used for total hip replacement surgery impact the choice of implant design and fixation method?
The surgical approach used for total hip replacement surgery may influence the choice of implant design and fixation method, as different approaches may require specific implant configurations or fixation techniques for optimal outcomes.
What are the differences between cemented and uncemented total hip replacement implants, and how do they affect the surgical procedure and recovery?
Cemented total hip replacement implants are fixed to the bone using bone cement, while uncemented implants rely on bone ingrowth for stability. The choice between cemented and uncemented implants depends on factors such as patient age, bone quality, and surgeon preference.
Can total hip replacement implants be made of biocompatible materials to reduce the risk of adverse reactions or implant rejection?
Yes, total hip replacement implants are typically made of biocompatible materials such as titanium alloys, cobalt-chromium alloys, ceramic, or polyethylene to minimize the risk of adverse reactions or implant rejection.
How does the size and shape of total hip replacement implants impact their stability and performance in the hip joint?
The size and shape of total hip replacement implants are carefully selected to match the patient’s anatomy and optimize stability and performance in the hip joint, reducing the risk of implant-related complications.
What are the advantages and disadvantages of metal-on-metal, metal-on-polyethylene, ceramic-on-ceramic, and ceramic-on-polyethylene total hip replacement implants?
Each combination of materials for total hip replacement implants has its advantages and disadvantages in terms of wear resistance, durability, friction, and potential for adverse reactions or complications.
How does the cost of total hip replacement implants vary depending on the type of material and design chosen?
The cost of total hip replacement implants varies depending on factors such as the type of material, design complexity, manufacturer, and any additional features or customization options.
Are there any specific precautions or follow-up care instructions for individuals with metal or ceramic total hip replacement implants?
Individuals with metal or ceramic total hip replacement implants may be advised to undergo regular follow-up appointments, monitoring for signs of implant wear or failure, and to report any unusual symptoms or discomfort promptly.
Can total hip replacement implants be MRI-compatible, or are there limitations for patients with implants undergoing imaging studies?
Some total hip replacement implants are MRI-compatible, while others may have limitations or contraindications for patients undergoing imaging studies. Patients should inform healthcare providers of any implants before undergoing MRI scans.
How do advancements in implant technology and materials influence the outcomes and longevity of total hip replacement surgery?
Advancements in implant technology and materials continue to improve the outcomes and longevity of total hip replacement surgery by enhancing implant durability, wear resistance, biocompatibility, and overall performance in the hip joint.
Can total hip replacement implants be used in patients with osteoporosis or compromised bone quality, or are there alternative options available?
Total hip replacement implants can be used in patients with osteoporosis or compromised bone quality, but special considerations may be necessary to ensure adequate implant fixation and stability. Alternative options such as bone grafting or specialized implant designs may be considered in some cases.
How do total hip replacement implants affect joint biomechanics and function compared to the natural hip joint?
Total hip replacement implants aim to restore joint biomechanics and function as closely as possible to the natural hip joint, allowing for improved mobility, pain relief, and quality of life in patients with hip joint disease.
What are the potential risks and benefits of using modular total hip replacement implants compared to non-modular designs?
Modular total hip replacement implants offer advantages such as intraoperative flexibility and customization but may also pose risks such as component loosening or fretting corrosion. The choice between modular and non-modular designs depends on factors such as patient anatomy and surgeon preference.
How does the choice of bearing surface in total hip replacement implants impact wear rates and long-term implant survival?
The choice of bearing surface in total hip replacement implants, such as metal-on-metal, metal-on-polyethylene, ceramic-on-ceramic, or ceramic-on-polyethylene, can influence wear rates and long-term implant survival, with each combination having unique characteristics and considerations.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
