Hip Bursitis
Hip bursitis is the inflammation of one or more bursae—small, fluid-filled sacs that cushion and reduce friction between muscles, tendons, and bones. In the hip, the two main bursae are the trochanteric bursa (on the side of the hip) and the iliopsoas bursa (in the front of the hip). When these bursae become irritated or inflamed, they can cause pain and limit movement. While the condition is usually not serious, it can cause significant discomfort and affect mobility.
How Common It Is and Who Gets It? (Epidemiology)
Hip bursitis is a common cause of hip pain, particularly among middle-aged and older adults. It tends to occur more often in women than in men and in individuals who participate in repetitive activities such as running, cycling, or climbing stairs. People with leg length differences, prior hip surgery, or conditions like rheumatoid arthritis are also at increased risk.
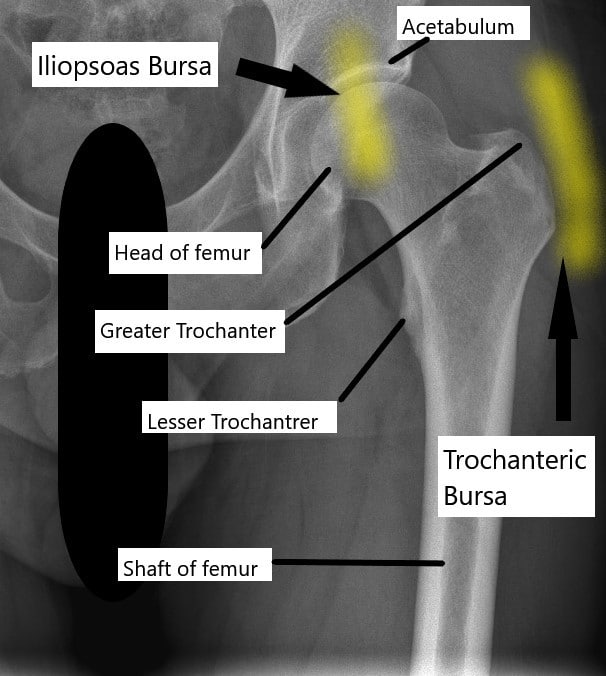
X-ray of the hip joint and its relation to the trochanteric bursa and iliopsoas bursa.
Trochanteric bursa
The trochanteric bursae is a small sac of fluid present at the side of the hip joint. The bursae allow the smooth gliding between the hip abductor muscles, tensor fascia, and the greater trochanter. The greater trochanter is bony prominence at the upper end of the thigh bone at the side of the hip joint.
Iliopsoas bursa
The iliopsoas bursa helps in the smooth gliding of the iliopsoas tendon over the front of the hip joint. The bursa may get inflamed and cause pain and tenderness. The pain is typically situated in front of the hip joint.
Why It Happens – Causes (Etiology and Pathophysiology)
Bursitis occurs when one or more of the hip bursae become inflamed due to irritation, injury, or overuse. Common causes include:
-
Direct trauma to the hip from a fall or impact.
-
Repetitive motion from activities like jogging or cycling, which can cause friction over the bursa.
-
Inflammatory diseases such as rheumatoid arthritis, which make bursae more prone to swelling.
-
Calcium deposits in nearby tendons that irritate the bursa.
-
Prior hip surgery or leg length differences, which alter joint mechanics and increase stress on the bursa.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint that connects the thigh bone (femur) to the pelvis. The trochanteric bursa lies between the greater trochanter (a bony prominence on the femur) and the muscles that move the hip. The iliopsoas bursa sits in front of the hip joint and allows smooth gliding of the iliopsoas tendon. These bursae reduce friction during movement, allowing pain-free motion of the hip and leg.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with trochanteric bursitis usually feel sharp or aching pain on the side of the hip that may spread down the thigh. Pain often worsens with walking, climbing stairs, or lying on the affected side.
Patients with iliopsoas bursitis typically feel pain in the front of the hip or groin. The pain may worsen when lifting the leg, walking uphill, or rising from a chair. In both types, discomfort is often worse at night.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a medical history and physical examination. The doctor will check for tenderness and reproduce the pain through specific movements. Imaging studies such as X-rays, CT scans, or MRI may be used to rule out other conditions like arthritis, fractures, or tendon injuries. Ultrasound can also help visualize inflammation in the bursa.
Classification
Hip bursitis is classified based on the affected bursa:
-
Trochanteric bursitis – Involves the outer side of the hip near the greater trochanter.
-
Iliopsoas bursitis – Involves the front of the hip near the groin.
Some patients may have both types at once, especially if hip mechanics are abnormal.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that can mimic hip bursitis include hip osteoarthritis, tendonitis, labral tears, lower back disorders, and referred pain from the spine or pelvis. Careful examination and imaging help differentiate these conditions.
Depo-Medrol used as a steroid shot in cortisone injection.
Treatment Options
Non-Surgical Care – Most cases respond well to conservative treatments:
-
Rest and modification of activities that worsen symptoms.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen for short-term relief.
-
Ice application to reduce inflammation and soothe pain.
-
Physical therapy to improve flexibility, strengthen surrounding muscles, and correct gait or posture issues.
-
Cortisone injections combining a steroid and local anesthetic (such as lidocaine) can provide lasting relief by reducing inflammation. Injections may be repeated if symptoms return.
Surgical Care – Surgery is rarely needed but may be considered for persistent cases that do not improve with conservative measures. Using minimally invasive arthroscopic techniques, the surgeon removes the inflamed bursa through small incisions. Patients can usually walk the same day and recover quickly.
Recovery and What to Expect After Treatment
Most patients improve within weeks of starting treatment. Pain relief from steroid injections may occur within a few days and last for months. Physical therapy helps restore strength and flexibility, reducing recurrence risk. Recovery after arthroscopic surgery is usually brief, with most patients returning to normal activities within a few weeks.
Possible Risks or Side Effects (Complications)
Potential complications include temporary soreness after injections, infection, bleeding, or, rarely, recurrence of bursitis. Long-term use of NSAIDs may cause stomach irritation or ulcers, so these medications are used carefully and for short periods.
Long-Term Outlook (Prognosis)
The prognosis for hip bursitis is excellent. Most patients recover fully with non-surgical treatment. Maintaining muscle strength and flexibility around the hip greatly reduces the chance of recurrence. Chronic cases may need periodic treatment or lifestyle modification.
Out-of-Pocket Costs
Medicare
CPT Code 20610 – Bursa Injection or Aspiration (Corticosteroid or Anesthetic Injection to Hip Bursa): $15.12
CPT Code 27062 – Open Trochanteric Bursectomy (Surgical Excision of Inflamed Trochanteric Bursa): $108.70
Medicare Part B generally covers 80% of the approved cost for these procedures once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield typically cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved procedures. These plans work alongside Medicare to fill the coverage gap and lower your financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it serves as a secondary payer. These plans usually cover any remaining coinsurance or small deductibles, which generally range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your trochanteric bursitis or hip inflammation is work-related, Workers’ Compensation will cover all associated medical expenses, including injections, surgery, rehabilitation, and follow-up visits. You will not have any out-of-pocket costs, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip bursitis developed due to an automobile accident or trauma, No-Fault Insurance will typically cover the total cost of treatment, including injections or bursectomy. The only potential out-of-pocket cost may be a small deductible or co-payment, depending on your insurance policy.
Example
Linda Walker was treated for chronic hip pain caused by trochanteric bursitis. She first received a bursa injection (CPT 20610) with an estimated Medicare out-of-pocket cost of $15.12. When symptoms persisted, she underwent an open trochanteric bursectomy (CPT 27062) with an estimated out-of-pocket cost of $108.70. Because Linda had supplemental insurance through AARP Medigap, her remaining balance was fully covered, leaving her with no out-of-pocket expenses for either procedure.
Frequently Asked Questions (FAQ)
Q. Is hip bursitis serious?
A. No. It’s usually a benign condition that responds well to rest, medication, or injections.
Q. Can I walk with hip bursitis?
A. Yes, but avoid overexertion. Gentle movement is encouraged, but stop if pain worsens.
Q. How long does recovery take?
A. Most people feel better within a few weeks, though some may need several months for full recovery.
Summary and Takeaway
Hip bursitis is a common, treatable cause of hip pain caused by inflammation of the bursae that cushion the joint. Most patients improve with rest, medication, and physical therapy. For persistent cases, a steroid injection or minimally invasive surgery may be needed. Maintaining hip strength and flexibility helps prevent recurrence.
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is typically managed by orthopedic surgeons, sports medicine specialists, or physiatrists. Physical therapists assist in rehabilitation, and radiologists may perform ultrasound-guided injections. Nurses and support staff help with pain management and post-procedure care.
When to See a Specialist?
If hip pain persists for more than two weeks, interferes with daily activities, or does not respond to home care, you should see an orthopedic specialist. Persistent tenderness or swelling near the hip also warrants evaluation.
When to Go to the Emergency Room?
Seek immediate care if you experience sudden severe hip pain after a fall, inability to bear weight, fever with hip swelling, or signs of infection such as redness or warmth at the injection site.
What Recovery Really Looks Like?
Early recovery involves rest and ice application. As pain improves, physical therapy helps restore strength and mobility. Most patients resume light activities within days and normal exercise within weeks, depending on the severity and treatment used.
What Happens If You Ignore It?
Ignoring hip bursitis can lead to chronic pain, stiffness, and weakness. Continued inflammation may affect surrounding muscles and tendons, limiting motion and increasing the risk of further injury.
How to Prevent It?
Preventive strategies include stretching before exercise, strengthening hip and core muscles, using proper footwear, and avoiding repetitive stress on the hips. Maintaining healthy posture and correcting leg length differences also help reduce strain.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and protein supports joint and bone health. Hydration and a balanced diet promote tissue repair and reduce inflammation. Avoiding excess alcohol and maintaining a healthy weight lessen joint stress.
Activity and Lifestyle Modifications
Low-impact activities such as swimming, yoga, and walking are ideal during recovery. Avoid running on hard surfaces or sitting for long periods. Gradual return to full activity, guided by a therapist, ensures lasting relief and prevents recurrence.
Do you have more questions?
What are the typical symptoms of hip bursitis, and how can I differentiate them from other hip-related conditions?
Understanding the specific symptoms of hip bursitis and how they differ from other hip conditions can help in accurate diagnosis and treatment planning. Your healthcare provider can provide guidance on distinguishing between various hip-related issues.
Is there a risk of developing chronic hip bursitis, and what steps can I take to prevent its recurrence?
Chronic hip bursitis is a possibility for some individuals, especially if underlying factors contribute to its development. Your healthcare provider can offer recommendations on preventive measures and lifestyle modifications to reduce the risk of recurrence.
Are there specific ergonomic or lifestyle changes I can make to alleviate hip bursitis symptoms during daily activities?
Modifying daily activities and ergonomics can help reduce strain on the hip joint and alleviate bursitis symptoms. Your healthcare provider or physical therapist can provide personalized recommendations based on your lifestyle and needs.
How long does it typically take to recover from hip bursitis, and what factors may influence the duration of recovery?
Recovery from hip bursitis can vary depending on individual factors such as the severity of inflammation, adherence to treatment, and underlying health conditions. Your healthcare provider can provide an estimate of the recovery timeline and factors that may affect it.
What are the potential side effects or risks associated with cortisone steroid injections for hip bursitis, and how common are they?
Cortisone steroid injections can provide relief from hip bursitis symptoms but may also carry risks or side effects. Understanding these potential complications can help you make informed decisions about treatment options. Your healthcare provider can discuss the risks and benefits of cortisone injections.
Are there any alternative or complementary therapies, such as acupuncture or chiropractic care, that may help alleviate hip bursitis symptoms?
Some individuals may find relief from hip bursitis symptoms through alternative or complementary therapies. Discussing these options with your healthcare provider can help determine if they are suitable for your situation and if they can be integrated into your treatment plan.
Can hip bursitis affect my ability to perform specific activities or sports, and are there modifications I should consider to prevent exacerbating the condition?
Hip bursitis may impact your ability to engage in certain activities or sports, depending on the severity of symptoms and underlying factors. Your healthcare provider can provide guidance on activity modifications to minimize discomfort and prevent worsening of the condition.
How can I manage pain and discomfort associated with hip bursitis at home, and are there specific self-care strategies I should follow?
Implementing self-care strategies at home can help manage pain and discomfort associated with hip bursitis. Your healthcare provider can provide guidance on effective home remedies, such as rest, ice therapy, and gentle stretching exercises.
Are there any specific warning signs or red flags that indicate a worsening of hip bursitis or the development of complications?
Being aware of potential warning signs or red flags can help you recognize when hip bursitis may be worsening or when complications may be developing. Your healthcare provider can provide guidance on what to watch for and when to seek medical attention.
What are the potential effects of hip bursitis on my mobility and daily activities, and how can I maintain independence during the recovery process?
Understanding how hip bursitis may affect mobility and daily activities can help you develop strategies to maintain independence during the recovery process. Your healthcare provider or physical therapist can provide guidance on adaptive techniques and assistive devices, if necessary.
Are there any dietary or nutritional recommendations that may help support healing and reduce inflammation associated with hip bursitis?
Certain dietary and nutritional factors may play a role in supporting healing and reducing inflammation associated with hip bursitis. Your healthcare provider or a registered dietitian can offer personalized recommendations based on your overall health and specific needs.
Can hip bursitis cause referred pain or discomfort in other areas of the body, and how can I distinguish between primary and referred pain?
Hip bursitis may sometimes cause referred pain or discomfort in other areas of the body, which can complicate diagnosis and treatment. Understanding the characteristics of primary and referred pain can help you and your healthcare provider differentiate between the two and identify the underlying cause of your symptoms.
What role does posture play in managing hip bursitis, and are there specific ergonomic adjustments I should make to alleviate symptoms?
Posture can impact hip bursitis symptoms, and making ergonomic adjustments may help alleviate discomfort. Your healthcare provider or a physical therapist can provide guidance on maintaining proper posture and making ergonomic modifications to your work or home environment.
Is there a risk of developing complications, such as infection or chronic inflammation, as a result of untreated or poorly managed hip bursitis?
Untreated or poorly managed hip bursitis may increase the risk of complications, including infection or chronic inflammation. Understanding these potential risks can underscore the importance of seeking timely treatment and adhering to recommended management strategies.
What steps can I take to optimize the effectiveness of physical therapy or rehabilitation exercises for hip bursitis, and how can I ensure proper technique and progression?
Maximizing the effectiveness of physical therapy or rehabilitation exercises is crucial for managing hip bursitis and promoting recovery. Your physical therapist can provide guidance on proper technique, progression of exercises, and strategies to optimize therapeutic outcomes.
Are there any specific precautions or limitations I should be aware of when engaging in physical activity or exercise to prevent exacerbating hip bursitis?
Understanding precautions and limitations when engaging in physical activity or exercise can help prevent exacerbation of hip bursitis symptoms. Your healthcare provider or physical therapist can provide personalized recommendations based on your condition and activity level.
What are the potential long-term implications of hip bursitis, and how can I minimize the risk of recurrence or complications over time?
Considering the potential long-term implications of hip bursitis can help you take proactive steps to minimize the risk of recurrence or complications. Your healthcare provider can offer guidance on lifestyle modifications, preventive measures, and ongoing management strategies to support long-term joint health.
Are there any alternative treatments or therapies, such as acupuncture, massage therapy, or herbal supplements, that may complement conventional medical approaches for managing hip bursitis?
Exploring alternative treatments or therapies alongside conventional medical approaches may provide additional relief for hip bursitis symptoms. Your healthcare provider can help evaluate the safety and efficacy of alternative therapies and incorporate them into your treatment plan, if appropriate.
How can I effectively communicate with my healthcare provider about my hip bursitis symptoms, treatment preferences, and concerns?
Effective communication with your healthcare provider is essential for optimizing your hip bursitis treatment and addressing any concerns or preferences you may have. Asking questions, expressing your needs, and actively participating in shared decision-making can help ensure that your treatment plan aligns with your goals and values.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
