Anterior Hip Replacement
Hip replacement surgery is considered one of the most successful operations in modern medicine. It offers significant relief from hip pain and stiffness, allowing patients to regain a lifestyle they enjoyed before the disease. The surgery involves replacing the damaged parts of the hip joint with artificial components to restore function and balance the muscular forces around the joint. Traditionally, hip replacement was performed using the posterior or lateral approach, but the newer anterior approach offers advantages such as faster recovery and less postoperative pain.
How Common It Is and Who Gets It? (Epidemiology)
Hip replacement surgery is common, with over 300,000 procedures performed annually in the U.S. It is most frequently performed in older adults with osteoarthritis, but younger patients with conditions like avascular necrosis, rheumatoid arthritis, or severe fractures also benefit from the procedure. The anterior approach has become increasingly popular due to its potential for quicker recovery times.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common reason for hip replacement is osteoarthritis, a degenerative condition that affects the cartilage in the hip joint. Other causes include:
-
Rheumatoid arthritis: A systemic condition that causes inflammation in the joint.
-
Avascular necrosis: Damage to the bone due to a loss of blood supply.
-
Hip fractures: Often resulting from falls or accidents, particularly in older adults.
These conditions lead to pain, stiffness, and a loss of function in the hip joint, affecting daily activities.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint made up of the femoral head (the ball) and the acetabulum (the socket in the pelvis). The ball is covered by smooth articular cartilage, which allows the joint to move freely. The muscles, ligaments, and tendons around the hip provide stability and facilitate movement such as walking, running, and sitting cross-legged.
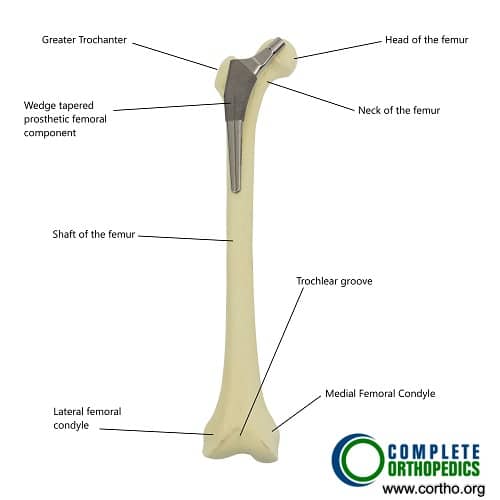
Normal hip anatomy and position of femoral stem in hip replacement surgery.
The ball is formed by the upper part of the thigh bone (femur), which fits into the cavity formed by the lower part of the pelvis (acetabulum). The ball and socket are covered by a smooth glistening white tissue known as articular cartilage. The articular cartilage helps in the smooth gliding of the joint in various movements of the joint such as walking, running, squatting, and sitting cross-legged.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with arthritis or other hip conditions experience:
-
Persistent pain: Felt in the groin, thigh, or buttocks, especially when walking or standing.
-
Stiffness: Difficulty moving the hip joint, such as bending, rotating, or sitting.
-
Reduced range of motion: Pain while trying to move the hip, which limits daily activities.
-
Pain at rest: Constant pain, especially at night, disrupting sleep.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
Physical exam: Assessment of the hip’s range of motion and stability.
-
X-rays: To check for joint space narrowing, bone spurs, and cartilage damage.
-
MRI or CT scans: To evaluate soft tissue damage and the severity of the condition.
Procedure Types or Techniques (Classification)
There are three common approaches for hip replacement surgery:
-
Anterior approach: The surgeon accesses the hip joint from the front, offering muscle-sparing benefits and a quicker recovery.
-
Posterior approach: The traditional method, where the surgeon operates from the back of the hip.
-
Lateral approach: The incision is made on the side of the hip.
The anterior approach for hip replacement
Traditionally, the surgery has been performed from behind known as the posterior approach or from the side known as the lateral approach. The more recent approach from the front, known as the anterior approach, promises a faster recovery with a decreased hospital stay.

Traditional posterior approach for hip replacement
The surgery is performed with the patient lying on his back under regional (spinal) or general anesthesia. A skin incision is made starting from the bony prominence in front of the pelvis towards the outer side of the kneecap.
In comparison to the posterior approach here, the tissues (muscles and tendons) are separated instead of being cut to reach the joint capsule.
Fewer tissues are separated from the thigh bone and pelvis compared to other approaches. Regardless of the approach, the necessary steps of replacing the diseased parts remain the same.
Arthritic bone is removed from the sides of the joint, and the ball of the femur is cut. The ball is removed to expose the socket.
- The damaged part of the acetabular socket is removed, and a cup made of metal alloy or ceramic is fixed with screws or press-fitted in the socket.
- A unique form of highly durable plastic called polyethylene is placed in the socket to allow smooth gliding
- A stem made of metallic alloy is inserted in the femur, which may be press-fit or fixed using a particular form of bone cement, allowing the bone to hold the implant.
- A prosthetic head made of metal alloy or ceramic is placed on the stem replacing the natural head of the femur.
- The prosthetic head is relocated back in the socket
- Skin and soft tissues are closed in layers, and a sterile dressing is placed on the wound
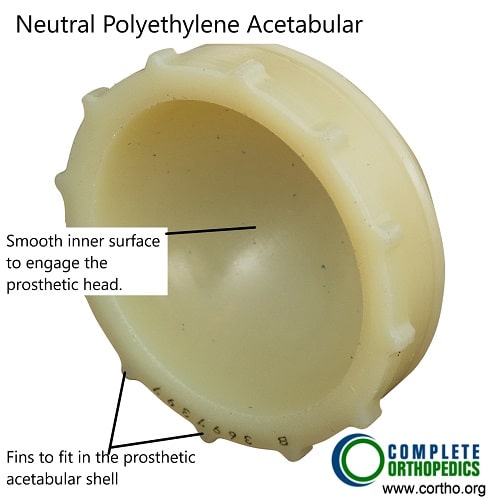
Neutral Polyethylene Acetabular Liner
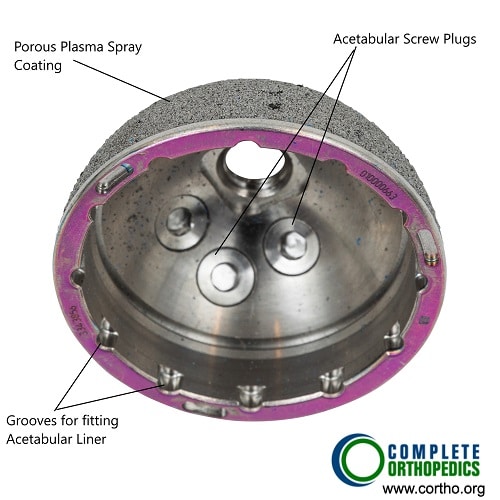
Acetabular Shell with screw holes and porous outer surface for bone ingrowth.
The acetabular shell may be made of cobalt chromium alloy and has a porous outer shell. The outer porous shell has a structure similar to bone trabeculae and aids in bone ingrowth. The ingrowth of bone allows a rigid fixation. The acetabular shell may also be fixed with acetabular screws that are carefully directed in the pelvic bone to prevent damage to neurovascular structures. The shell is lined by a liner which is made of highly cross linked polyethylene. The cross linking is achieved using radiation and the polyethylene is then treated with anti-oxidants to prevent wear and tear damage.
Benefits of anterior approach
The anterior approach is also known as the “muscle-sparing hip arthroplasty,” has several benefits over the traditionally performed posterior approach.
- In the inter-muscular approach, fewer muscles are damaged during the procedure. The Hip abductors and IT band muscles are spared, which are traditionally cut in other approaches.
- There is less postoperative pain owing to fewer muscles being damaged therefore decreasing the need for postoperative analgesics
- Faster recovery is possible as fewer tissues are damaged. The patients can walk bearing weight with crutches after the anesthesia wears off in a few hours. In some cases, the patients can go home the day of surgery.
- The joint is more superficial in the front giving the surgeon the ability to reach the joint more easily without cutting through layers of tissue in the back.
- The approach provides excellent exposure of the socket, helping in proper placement of the components.
- There is an added advantage to using X-ray during the surgery, aiding the surgeon in proper placement of the implant. Correct placement of implants prevent complications such as leg length discrepancies and assures maximum longevity of the implant.
- In cases where both the hips are needed to be replaced in a single surgery, the anterior approach offers a straightforward approach to the other Hip without changing positions.
- Less postoperative complications such as hip dislocation in case of an anterior approach
- Fewer postoperative restrictions in case of anterior Hip replacement
Candidates for anterior hip replacement
Not everyone is a candidate for the anterior approach of Hip replacement. Large/obese/muscular patients are generally approached with more traditional approaches.
Hip pain due to arthritis remains the most common indication for hip replacement. Chronic hip pain not relieved by conservative/nonsurgical management such as weight loss, diet, exercise, medications (Tylenol and Anti-Inflammatory), intra-articular injections, physical therapy, and assistive devices. Hip pain can be due to several causes
- Osteoarthritis is also known as wear, and tear arthritis is common in the elderly population but can also affect the younger age group due to trauma or sports injuries. The risk factors for osteoarthritis are age, obesity, genetics, diet, and sedentary lifestyle.
- Childhood hip joint infections and a growing hip joint mismatch can lead to chronic hip pain.
- Inflammatory and metabolic systemic disorders such as rheumatoid arthritis and gout generally affect both the hip joints. Rheumatoid arthritis is a medical condition where the body’s cells destroy the structures forming the joint.
- Osteonecrosis or avascular necrosis leads to the destruction of the Hip joint as a result of damaged or reduced blood supply.
Challenges in anterior hip replacement
The anterior approach to the hip joint has a steep learning curve being technically difficult. The surgical approach also has a problematic exposure to place femoral stem. It is also challenging to address intraoperative complications with increased blood loss.
Some patients report numbness over the outer surface of the thigh as a nerve supplying the part can be pressed or cut during the approach. The approach also becomes challenging to perform in the case of large and obese patients or patients with deformities.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that may mimic hip arthritis include:
-
Trochanteric bursitis: Inflammation of the bursa near the hip.
-
Piriformis syndrome: Compression of the sciatic nerve by the piriformis muscle.
-
Hip labral tears: Damage to the cartilage around the hip socket.
-
Lumbar radiculopathy: Nerve pain from the lower back affecting the hip area.
Treatment Options
Before surgery, conservative treatments are recommended, including:
-
Physical therapy to strengthen the muscles around the hip.
-
Medications: Pain relievers and anti-inflammatory drugs.
-
Assistive devices: Canes or walkers to help with mobility.
If these measures fail to provide relief, hip replacement surgery is considered.
Recovery and What to Expect After Surgery
-
Post-surgery care: Patients will wear a sling or immobilizer to protect the hip while it heals.
-
Physical therapy: Starts soon after surgery to help regain movement and strength.
-
Pain relief: Most patients experience significant pain reduction within weeks of surgery.
-
Full recovery: Takes approximately 3–6 months, with most patients returning to daily activities after 3 months.
Possible Risks or Side Effects (Complications)
-
Infection and blood clots are potential risks after surgery.
-
Dislocation of the hip joint, particularly in the initial recovery period.
-
Leg length discrepancy: A slight difference in leg length post-surgery.
-
Persistent pain or stiffness may occur in rare cases.
Long-Term Outlook (Prognosis)
Most patients experience significant pain relief and improved mobility. Hip replacements typically last 15–20 years or longer, depending on the patient’s activity level and the quality of the implant. Patients are encouraged to maintain a healthy weight and engage in low-impact activities to preserve the longevity of the implant.
Out-of-Pocket Cost
Medicare
CPT Code 27130 – Anterior Hip Replacement (Total Hip Arthroplasty via the Anterior Approach): $303.45
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans typically cover any remaining coinsurance or small deductibles, which generally range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your anterior hip replacement is required due to a work-related injury or repetitive trauma, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only possible out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Kevin Mitchell underwent anterior hip replacement (CPT 27130) after years of hip arthritis. His estimated Medicare out-of-pocket cost was $303.45. Since Kevin had supplemental insurance through AARP Medigap, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How long will my hip replacement last?
A. Most implants last 15–20 years.
Q. Can I return to sports after surgery?
A. Low-impact activities like swimming, walking, and cycling are encouraged, while high-impact activities like running should be avoided.
Q. When can I return to work?
A. Patients with sedentary jobs can return in 2–4 weeks, while physically demanding jobs may require 6–12 weeks.
Summary and Takeaway
Hip replacement surgery is highly effective in reducing pain and restoring mobility for patients suffering from arthritis or injury. The anterior approach offers numerous advantages, including faster recovery and less postoperative pain.
Clinical Insight & Recent Findings
For patients undergoing total hip replacement (THR), surgery via the direct anterior approach (DAA) has been shown to offer numerous benefits, such as faster recovery and less postoperative pain.
A recent study compared two techniques used during THR surgery: the traditional “on-table” method using an orthopedic traction table and the “off-table” method using a standard operating table. The study found that transitioning to the off-table technique resulted in a 43-minute reduction in total room time, improving overall operating room efficiency.
This transition, which does not compromise surgical outcomes, allows for increased surgical throughput, potentially enabling more surgeries per day and improving resource management in busy surgical centers. (“Study on the benefits of the off-table technique in hip replacement surgery – see PubMed.“)
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in joint replacements perform the surgery, assisted by anesthesiologists, nurses, and physical therapists.
When to See a Specialist?
If you experience persistent hip pain that interferes with daily activities or if you have limited mobility, consult with an orthopedic surgeon to evaluate whether surgery is needed.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience severe pain, signs of infection, or if you cannot move your hip after surgery.
What Recovery Really Looks Like?
The first 6 weeks involve pain management and gentle movement exercises. Most patients experience significant pain relief and improved mobility, with full recovery typically achieved within 3–6 months.
What Happens If You Delay Surgery?
Delaying surgery may result in worsening pain, further loss of mobility, and a decreased quality of life. Surgical intervention can prevent these complications.
How to Prevent Recurrence or Failure?
Maintain strength around the hip joint through rehabilitation and avoid high-impact activities. Regular follow-ups with your surgeon will ensure the implant remains functional.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and protein promotes bone healing and supports joint health. Avoid smoking and limit alcohol intake for optimal recovery.
Activity and Lifestyle Modifications
Engage in low-impact exercises such as swimming and walking, and avoid high-impact activities that can stress the implant.
Do you have more questions?
Can anterior hip replacement surgery be performed on patients with hip dysplasia or developmental abnormalities?
Anterior hip replacement surgery may be feasible for some patients with hip dysplasia or developmental abnormalities, but careful evaluation by an orthopedic surgeon experienced in complex hip reconstruction is necessary to determine the most appropriate surgical approach and implant selection.
Are there any specific recommendations for preventing falls or injuries during the recovery period?
Patients are advised to take precautions such as keeping walkways clear of obstacles, using assistive devices as needed, and following prescribed activity restrictions to minimize the risk of falls or injuries during the recovery period.
How is pain managed during the rehabilitation process after anterior hip replacement surgery?
Pain management during rehabilitation may include a combination of medications, physical therapy modalities such as ice therapy or transcutaneous electrical nerve stimulation (TENS), and gentle stretching and strengthening exercises to promote healing and mobility.
What types of assistive devices or aids are recommended during the recovery period after anterior hip replacement surgery?
Assistive devices such as walkers, crutches, or canes may be used initially to aid mobility and prevent falls during the early recovery phase. Gradual transition to walking aids and eventual independence is typically encouraged with ongoing rehabilitation.
Can patients with previous hip surgeries undergo anterior hip replacement surgery?
In many cases, patients with previous hip surgeries may still be candidates for anterior hip replacement surgery. However, the decision depends on factors such as the nature of the previous surgeries, hip anatomy, and the patient’s overall health.
Are there any lifestyle modifications or adaptations needed for patients after anterior hip replacement surgery?
While most patients can resume their usual activities after anterior hip replacement, modifications such as avoiding high-impact sports and maintaining a healthy weight may be recommended to prolong implant longevity and optimize outcomes.
What factors might indicate the need for revision surgery following anterior hip replacement?
Factors such as persistent pain, implant loosening or wear, instability, or component malposition may necessitate revision surgery. Regular follow-up appointments and monitoring of implant function are essential for early detection of potential issues.
How soon after surgery can patients resume normal activities such as driving and household chores?
The timing for resuming normal activities varies among patients and depends on factors such as surgical approach, individual healing, and postoperative rehabilitation progress. Patients should follow their surgeon’s guidance regarding activity progression.
Can anterior hip replacement surgery be performed on patients with osteoporosis?
Anterior hip replacement surgery can be performed on patients with osteoporosis, but careful consideration of bone quality and potential implant stability is necessary. Bone density assessments and consultation with a bone health specialist may be warranted in such cases.
Are there any restrictions on bending, twisting, or lifting following anterior hip replacement surgery?
Initially, patients are advised to avoid excessive bending or twisting of the hip joint and heavy lifting to prevent strain on the surgical site. Specific activity restrictions may vary depending on individual patient factors and surgical outcomes.
What measures are taken to minimize postoperative pain and discomfort after anterior hip replacement surgery?
Various pain management techniques are employed, including regional anesthesia, oral or intravenous pain medications, and non-pharmacological interventions such as ice therapy and positioning aids. Multimodal pain management approaches are often used to optimize patient comfort.
How are patients monitored for complications during the recovery period after anterior hip replacement surgery?
Patients are closely monitored postoperatively for signs of complications such as infection, blood clots, or implant instability. Regular follow-up appointments and imaging studies may be conducted to assess healing and implant function.
Can anterior hip replacement surgery be performed on patients with severe hip deformities or abnormalities?
Anterior hip replacement surgery may be feasible for some patients with severe hip deformities or abnormalities, but careful preoperative planning and assessment are necessary to ensure optimal outcomes.
What are the potential long-term effects or complications of anterior hip replacement surgery?
Long-term complications may include implant wear, loosening, or dislocation, which could necessitate revision surgery. However, with proper implant selection, surgical technique, and postoperative care, the risk of complications is minimized.
How long do patients typically stay in the hospital following anterior hip replacement surgery?
Hospital stays vary but are often shorter compared to traditional approaches, typically ranging from 1 to 3 days. Early mobilization and rehabilitation are key components of the recovery process.
Can anterior hip replacement surgery be performed on patients with metal allergies?
Alternative implant materials may be available for patients with metal allergies, allowing anterior hip replacement surgery to be safely performed while minimizing the risk of allergic reactions.
What type of anesthesia is typically used for anterior hip replacement surgery, and are there any alternatives?
Regional anesthesia (e.g., spinal or epidural) or general anesthesia are commonly used. Patient factors and preferences are considered when selecting the most appropriate anesthesia method.
Are there any dietary supplements or vitamins recommended to support healing after anterior hip replacement surgery?
While not universally prescribed, supplements such as vitamin D and calcium may support bone health and aid in the healing process. However, individual patient needs should be assessed.
How soon after surgery can patients expect to see improvement in their hip pain and mobility?
Many patients experience immediate relief from hip pain following surgery. Improvement in mobility typically progresses over several weeks as swelling decreases and tissues heal.
What measures are taken to prevent infection during and after anterior hip replacement surgery?
Strict adherence to sterile surgical techniques, antibiotic prophylaxis before surgery, and meticulous wound care postoperatively are essential in minimizing the risk of infection.
Are there any specific exercises or activities to avoid after anterior hip replacement surgery?
Initially, patients should avoid high-impact activities and strenuous exercises that put excessive stress on the hip joint. Physical therapy will guide patients on appropriate exercises for rehabilitation.
Can anterior hip replacement surgery be performed on patients with hip fractures?
In certain cases, anterior hip replacement can be performed on patients with hip fractures, depending on the fracture type and patient’s overall health. It’s essential to assess each case individually to determine the most suitable approach.
What are the potential risks or complications specific to anterior hip replacement surgery?
Potential risks include injury to nearby nerves and blood vessels, increased risk of fracture during surgery, and implant malpositioning. However, these risks are minimized with careful surgical technique and proper patient selection.
How does the recovery time for anterior hip replacement compare to traditional approaches?
Recovery time for anterior hip replacement is typically shorter compared to traditional approaches due to less disruption of muscles and soft tissues. Patients often experience faster mobilization and return to normal activities.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
