Core Decompression for Avascular Necrosis of the Hip
Core decompression is a surgical procedure designed to treat early-stage avascular necrosis (AVN) of the femoral head. Avascular necrosis, also known as osteonecrosis, occurs when the blood supply to the bone is disrupted, leading to bone death. Core decompression involves creating small tunnels in the femoral head to reduce internal pressure, stimulate revascularization, and prevent further bone collapse, helping to preserve the hip joint and delay the need for joint replacement surgery.
How Common It Is and Who Gets It? (Epidemiology)
Avascular necrosis is relatively common in individuals aged 30–60, with the condition affecting both men and women. Common causes include corticosteroid use, alcoholism, trauma, and systemic diseases like rheumatoid arthritis or lupus. It often affects the hip joint and can lead to debilitating pain and mobility loss if not treated.
Why It Happens – Causes (Etiology and Pathophysiology)
Avascular necrosis occurs when the blood supply to the femoral head (ball of the hip joint) is compromised. This leads to the death of bone tissue, weakening the bone structure and causing it to collapse. Without proper blood flow, the bone’s natural repair processes cannot function, resulting in cartilage damage, joint degeneration, and arthritis. Risk factors for AVN include prolonged corticosteroid use, excessive alcohol consumption, trauma, and certain medical conditions like sickle cell anemia or deep-sea diving.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint composed of the femoral head (ball) and the acetabulum (socket) in the pelvis. The femoral head is covered by a smooth layer of articular cartilage, which allows for frictionless movement within the acetabulum. Blood flow to the femoral head is provided by the medial and lateral circumflex arteries, which supply nutrients and oxygen to the bone. When this blood flow is disrupted, the bone tissue begins to deteriorate.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms of avascular necrosis include:
-
Hip pain: Typically in the groin or outer hip, often worsened by weight-bearing activities.
-
Stiffness: Difficulty with range of motion, especially with bending or rotating the hip.
-
Pain at rest: In more advanced cases, pain can occur even when not moving.
-
Limping: Due to weakness in the joint, leading to difficulty walking.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
Physical exam: The doctor may assess hip movement, tenderness, and pain response.
-
X-rays: Early stages of AVN may not show on X-rays, but in advanced stages, joint collapse or bone sclerosis may be visible.
-
MRI or bone scan: These imaging techniques provide a clearer picture of bone damage and early-stage AVN, identifying changes before they show up on X-rays.
Procedure Types or Techniques (Classification)
Core decompression involves creating one or multiple tunnels in the femoral head to relieve internal pressure and stimulate blood flow. Variations of the procedure include:
-
Autograft core decompression: The use of bone marrow or bone grafts from the patient’s body.
-
Allograft core decompression: The use of donor tissue for grafting.
The procedure involves the creation of a small tunnel/tunnels in the head of the femur to slow or stop the osteonecrosis. The patient is laid on the operating table and the leg is placed in a specially designed table for positioning.
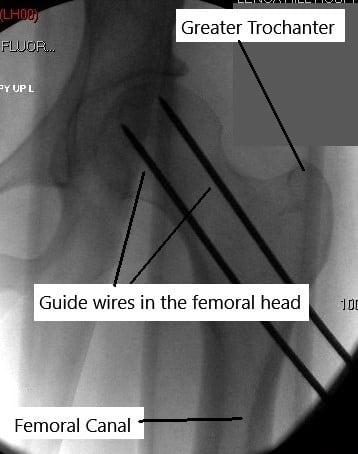
An intraoperative X-ray known as C-arm is used for checking the position of the instruments during the surgery. The patient may be given an intravenous sedative, spinal anesthesia, or general anesthesia. A small incision is given on the outer side of the upper thigh.
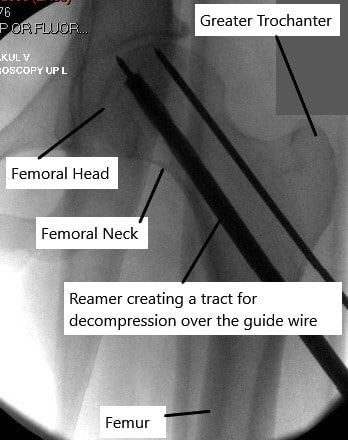
A small guide wire is passed from the incision to reach the area of the avascular necrosis without breaching the articular cartilage. A small drilling instrument is passed over the guidewire to create a tunnel to the dead bone. The procedure may involve the use of multiple drill holes instead of a single hole.
Usually, bone marrow is injected through the hole in the area of the dead bone. Sometimes bone graft taken from the patient’s body or from a bone bank may be used to fill the tunnel. The incision is closed with a suture and sterile dressing is placed on the site. The creation of a tunnel/tunnels decreases the pressure inside the head of the femur.
The reduction of pressure may lead to revascularisation and therefore repair the area of nonviable bone. The addition of bone marrow or bone graft may provide stem cells which may lead to early repair of the dead bone.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Osteoarthritis: Can present with similar pain and stiffness, but it generally affects the entire joint and is seen in older adults.
-
Hip labral tear: Often causes pain in the groin and a clicking sensation, but labral tears are more commonly associated with younger patients.
-
Trochanteric bursitis: Inflammation of the bursa on the outer hip, which may mimic AVN in terms of location and symptoms.
Treatment Options
-
Conservative management: Includes pain relievers, physical therapy, and weight management to reduce stress on the hip joint.
-
Core decompression surgery: Performed when conservative treatments fail and the patient is in the early stages of AVN (stages 1 and 2 of the Ficat & Arlet classification).
-
Hip replacement surgery: In advanced stages of AVN, joint replacement may be required if core decompression is ineffective.
Recovery and What to Expect After Surgery
-
Postoperative care: Patients typically wear a brace or crutches to limit weight-bearing for 4–6 weeks after surgery.
-
Physical therapy: Rehabilitation starts with passive exercises and progresses to active strengthening exercises after 6 weeks.
-
Return to activities: Most patients can return to low-impact activities, such as walking or swimming, within 3–6 months. High-impact activities should be avoided.
Possible Risks or Side Effects (Complications)
-
Infection: As with any surgery, there is a risk of infection at the incision site.
-
Fracture: If the bone fails to revascularize, it can collapse, requiring further intervention.
-
Graft failure: In some cases, the bone graft may not heal properly, leading to persistent pain or need for revision surgery.
Long-Term Outlook (Prognosis)
Core decompression has a high success rate when performed in the early stages of AVN. Many patients experience reduced pain and improved function for several years. However, the condition may progress in some cases, and hip replacement surgery may eventually be needed.
Out-of-Pocket Cost
Medicare
CPT Code 27071 – Core Decompression for Avascular Necrosis of the Hip: $228.82
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans typically cover any remaining balance, including coinsurance or small deductibles, which generally range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your core decompression surgery for avascular necrosis is work-related, Workers’ Compensation will cover all medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip avascular necrosis is related to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only possible out-of-pocket cost may be a small deductible or co-payment depending on your policy.
Example
Steven Clark required core decompression (CPT 27071) to treat avascular necrosis in his hip. His estimated Medicare out-of-pocket cost was $228.82. Since Steven had supplemental insurance through Blue Cross Blue Shield, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. How long will the benefits last?
A. Core decompression can provide symptom relief for several years, though some patients may eventually require a hip replacement.
Q. Will I be able to return to sports?
A. Patients can often return to low-impact sports, but high-impact activities should be avoided.
Q. Is it painful?
A. Most patients experience mild to moderate discomfort after surgery, which subsides with physical therapy and pain management.
Summary and Takeaway
Core decompression is an effective, minimally invasive procedure for early-stage avascular necrosis, offering a chance to avoid or delay hip replacement surgery. With proper patient selection, it can relieve pain, restore function, and improve quality of life.
Clinical Insight & Recent Findings
Core decompression is a well-established treatment for early-stage avascular necrosis (AVN) of the hip, aiming to prevent further bone collapse and delay the need for joint replacement.
A recent study explored an advanced method of performing core decompression using hip arthroscopy alongside bone grafting. This technique involves using an expandable reamer to decompress the necrotic femoral head while maintaining minimal disruption to healthy bone.
The study found that combining core decompression with hip arthroscopy not only improves the precision of the procedure but also addresses accompanying joint pathologies such as labral tears. Additionally, bone grafting with autologous and allogeneic materials enhances healing, contributing to long-term joint stability. (“Study on arthroscopy-assisted core decompression for AVN of the hip – see PubMed.“)
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in hip and joint reconstruction perform core decompression surgery, often in collaboration with physical therapists and anesthesiologists.
When to See a Specialist?
Consult an orthopedic specialist if you experience persistent hip pain, difficulty walking, or reduced range of motion, especially if you have a history of trauma, corticosteroid use, or alcohol consumption.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience severe hip pain, fever, or signs of infection after surgery.
What Recovery Really Looks Like?
Recovery involves a gradual return to mobility, with most patients seeing significant improvement within 3–6 months. Physical therapy is key to regaining strength and function.
What Happens If You Delay Surgery?
Delaying core decompression may lead to further progression of AVN, resulting in joint collapse and the need for more invasive surgeries like total hip replacement.
How to Prevent Recurrence or Failure?
Maintain a healthy weight, avoid high-impact activities, and continue physical therapy to ensure the best outcome.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D supports bone health and healing. Proper hydration and avoiding smoking can further promote recovery.
Activity and Lifestyle Modifications
After surgery, engage in low-impact exercises like swimming or walking to maintain joint health, and avoid heavy lifting or running to protect the hip.
Do you have more questions?
Are there any alternative or complementary therapies that patients can explore alongside traditional medical treatments for avascular necrosis of the hip?
What steps can patients take to optimize their recovery and improve the success of core decompression surgery?
Following post-operative instructions, maintaining a healthy lifestyle, attending physical therapy sessions, and attending follow-up appointments are essential for optimal recovery.
Is avascular necrosis of the hip more prevalent in certain demographic groups or populations with specific genetic predispositions?
Certain genetic factors may predispose individuals to avascular necrosis, but the condition can occur in people of all demographics.
What are the typical costs associated with core decompression surgery, and does insurance typically cover the procedure?
Costs can vary depending on factors such as hospital fees, surgeon fees, and post-operative care, and insurance coverage may vary based on individual policies.
Are there any occupational or lifestyle modifications that patients should consider after undergoing core decompression surgery?
Depending on their occupation and activities, patients may need to avoid high-impact or strenuous activities to protect the hip joint and aid in recovery.
How often should patients undergo follow-up imaging or clinical evaluations after core decompression surgery to monitor disease progression?
Follow-up frequency may vary but is typically every few months initially, then less frequently if the disease remains stable.
What are the potential complications associated with long-term use of medications to manage avascular necrosis symptoms, such as nonsteroidal anti-inflammatory drugs (NSAIDs)?
Long-term NSAID use may increase the risk of gastrointestinal bleeding, kidney damage, and cardiovascular events, so careful monitoring is necessary.
Are there any emerging treatments or research advancements in the field of avascular necrosis that patients should be aware of?
Research into new treatment modalities, such as stem cell therapy or biologic agents, is ongoing, but further studies are needed to assess their efficacy and safety.
How does avascular necrosis of the hip affect a patient’s quality of life, particularly in terms of mobility and pain management?
Avascular necrosis can significantly impact mobility and cause chronic pain, affecting daily activities and overall quality of life.
Are there any specific rehabilitation exercises or physical therapy regimens recommended after core decompression surgery?
Yes, physical therapy plays a crucial role in recovery and may include exercises to improve hip strength, flexibility, and range of motion.
What are the long-term outcomes of core decompression surgery compared to other surgical interventions, such as total hip replacement?
Long-term outcomes can vary, but core decompression may delay or avoid the need for hip replacement in some patients, while others may eventually require joint replacement.
Can core decompression surgery be performed bilaterally (on both hips) simultaneously, or is it typically done one hip at a time?
Bilateral core decompression surgery can be performed in select cases, but the decision depends on factors such as the patient’s overall health and surgical risk.
What are the factors that determine whether a patient is a suitable candidate for core decompression surgery?
Factors such as the stage of avascular necrosis, the extent of bone damage, overall health, and lifestyle factors are considered when determining candidacy for core decompression.
Are there any dietary or nutritional recommendations that can support bone health and potentially reduce the risk of avascular necrosis recurrence?
Maintaining a balanced diet rich in calcium and vitamin D may support bone health, but specific dietary recommendations may vary based on individual factors.
Is core decompression surgery appropriate for all patients with avascular necrosis of the hip, regardless of disease stage?
Core decompression is typically recommended for early-stage avascular necrosis, and its effectiveness may diminish as the disease progresses.
Can avascular necrosis of the hip be managed with non-surgical treatments alone?
In early stages, non-surgical treatments such as medication, physical therapy, and lifestyle modifications may help manage symptoms.
How does core decompression surgery differ from other treatment options for avascular necrosis?
Core decompression involves creating tunnels in the femoral head to relieve pressure and stimulate bone repair, whereas other options may include medication or joint replacement.
What are the success rates of core decompression surgery in preventing the progression of avascular necrosis?
Success rates vary depending on the stage of the disease and individual factors, but early intervention with core decompression can significantly slow or halt disease progression.
How long does it typically take to recover from core decompression surgery?
Recovery can vary, but patients typically begin weight-bearing activities within a few weeks and may return to normal activities within a few months.
What are the success rates of core decompression surgery in preventing the progression of avascular necrosis?
Success rates vary depending on the stage of the disease and individual factors, but early intervention with core decompression can significantly slow or halt disease progression.
How long does it typically take to recover from core decompression surgery?
Recovery can vary, but patients typically begin weight-bearing activities within a few weeks and may return to normal activities within a few months.
Are there any potential complications associated with core decompression surgery?
Complications are rare but can include infection, bleeding, or failure to relieve symptoms if the disease is advanced.
What imaging tests are used to diagnose avascular necrosis of the hip?
X-rays, MRI scans, and bone scans are commonly used to diagnose avascular necrosis and assess the extent of bone damage.
What are the limitations of core decompression surgery in treating advanced stages of avascular necrosis?
Core decompression may be less effective in advanced stages when significant bone collapse has occurred, and joint replacement surgery may be necessary.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
