Direct Anterior Total Hip Arthroplasty
Anterior hip replacement is a cutting-edge surgical procedure that has gained popularity due to its muscle-sparing approach. Unlike traditional hip replacements, which are performed through the posterior or lateral approaches, the anterior approach allows surgeons to access the hip joint from the front, reducing the disruption of muscles and tendons. This technique promotes faster recovery and less postoperative pain.
How Common It Is and Who Gets It? (Epidemiology)
Hip replacement surgery is commonly recommended for patients with moderate to severe hip arthritis. It’s especially beneficial for patients in their 50s and 60s, although it can be performed on younger, active individuals or older patients with good health. The anterior approach is particularly suited for individuals with a lower BMI and those without a large abdominal pannus.
Why It Happens – Causes (Etiology and Pathophysiology)
Hip arthritis, the most common cause for hip replacement, develops due to the breakdown of cartilage in the hip joint, leading to pain and stiffness. Non-traumatic causes such as age, obesity, and long-term wear-and-tear are common. Trauma and other conditions like osteonecrosis can also lead to the need for a hip replacement.
How the Body Part Normally Works? (Relevant Anatomy)
The hip is a ball-and-socket joint. The ball is formed by the femoral head (top of the thigh bone), and the socket is part of the pelvis called the acetabulum. Healthy articular cartilage covers these surfaces, enabling smooth, pain-free movement. The hip joint supports weight and facilitates a wide range of motion, including walking, running, and sitting.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with advanced hip arthritis typically experience:
-
Pain: In the groin, outer thigh, or buttocks.
-
Stiffness: Difficulty with bending, squatting, and walking.
-
Loss of mobility: Reduced ability to perform daily activities.
-
Pain at rest: In some cases, pain persists even when not bearing weight on the hip.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
Physical examination: The doctor assesses pain, stiffness, and the range of motion.
-
X-rays: Usually the first imaging test, showing joint space narrowing and bone changes.
-
MRI or CT scan: Can provide more detail, especially if there are concerns about soft tissue or other joint structures.
Procedure Types or Techniques (Classification)
-
Direct Anterior Hip Replacement: The surgeon accesses the joint from the front, using specialized equipment to spare muscles and tendons.
-
Posterior Hip Replacement: A more traditional approach, where the muscles around the hip joint are cut to access the hip.
-
Lateral Hip Replacement: Involves a surgical approach from the side.
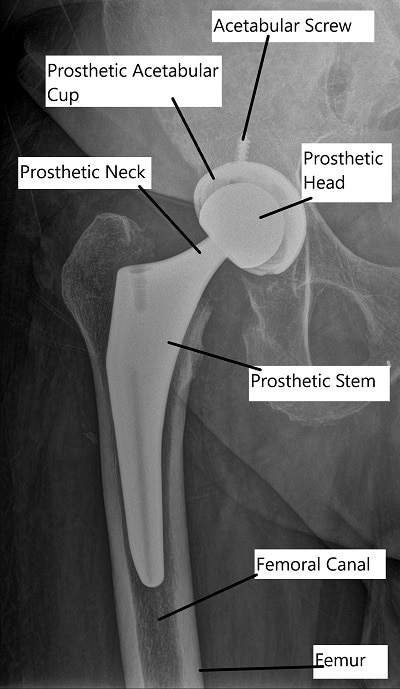
X-ray showing Total Hip Replacement in AP view.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Trochanteric bursitis: Inflammation of the bursa on the outside of the hip, causing pain in the same region.
-
Labral tears: Can cause hip pain and stiffness, but is more commonly seen in younger patients.
-
Lower back issues: Problems in the lumbar spine can mimic hip pain, especially when radiating down the leg.
Treatment Options
-
Non-surgical: Includes physical therapy, pain management with medications (e.g., NSAIDs, acetaminophen), and weight loss.
-
Surgical: Hip replacement surgery is considered when non-surgical treatments fail. The anterior approach is preferred for its quicker recovery time.
Recovery and What to Expect After Surgery
-
First few days: Patients may start weight-bearing with crutches or a walker. Most can go home the same day or the following day.
-
First month: Physical therapy begins to improve mobility and strength.
-
Long-term recovery: Most patients achieve full recovery in 3-6 months, with some returning to work and recreational activities sooner.
Possible Risks or Side Effects (Complications)
-
Infection: A risk with any surgery, though the anterior approach has fewer complications compared to the posterior approach.
-
Hip dislocation: Rare, but possible in the early recovery stages.
-
Nerve injury: Especially around the hip and thigh area.
-
Blood clots: A potential risk that can be managed with medication and physical activity.
Long-Term Outlook (Prognosis)
-
Most patients experience significant pain relief and improved hip function.
-
Hip replacement implants typically last 15-20 years, with many patients not requiring revision surgery for several decades.
-
Younger patients may need a revision in the future, but modern implants are designed for durability.
Out-of-Pocket Cost
Medicare
CPT Code 27130 – Direct Anterior Total Hip Arthroplasty (THA, Total Hip Replacement via the Anterior Approach): $303.45
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce patient costs.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it serves as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which usually range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your direct anterior THA is required due to a work-related injury or degenerative joint disease, Workers’ Compensation will cover all medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
John Doe required direct anterior THA (CPT 27130) after years of hip arthritis. His estimated Medicare out-of-pocket cost was $303.45. Since John had supplemental insurance through Blue Cross Blue Shield, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How long does it take to recover?
A. Full recovery usually takes 3-6 months, though many patients can return to low-impact activities in a few weeks.
Q. Can I walk after surgery?
A. Yes, most patients begin walking with crutches or a walker the same day as surgery.
Q. What activities can I do post-surgery?
A. Low-impact activities like swimming, biking, and walking are encouraged, while high-impact sports should be avoided.
Summary and Takeaway
Anterior hip replacement is a safe and effective surgery for patients with severe hip arthritis. It offers quicker recovery, less pain, and fewer complications compared to traditional approaches. If you’re a candidate for this surgery, consult with an orthopedic surgeon to discuss the best approach for your specific needs.
Clinical Insight & Recent Findings
The direct anterior approach (DAA) for total hip arthroplasty (THA) has gained popularity for its minimally invasive nature, allowing for faster recovery compared to traditional approaches. A recent study focused on its use in treating displaced femoral neck fractures (FNFs) in patients with dementia.
By utilizing a dual mobility cup (DMC), the study found no postoperative dislocations after one year in both dementia and non-dementia groups. Additionally, although functional recovery was similar between the two groups, dementia patients in non-rehabilitation settings showed greater declines in mobility, suggesting the importance of rehabilitation for these patients.
This study supports the effectiveness of DAA-THA with DMC in dementia patients, providing good outcomes for femoral neck fractures. (“Study on the use of direct anterior hip replacement with dual mobility cup for femoral neck fractures in dementia patients – see PubMed.“)
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons with expertise in hip replacements, particularly those trained in the anterior approach, perform this surgery. The surgical team may also include anesthesiologists, surgical assistants, and physical therapists.
When to See a Specialist?
If you’re experiencing persistent hip pain, stiffness, or difficulty with daily activities, consult with an orthopedic surgeon to explore your surgical options.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience sudden, severe hip pain, or if you notice signs of infection (fever, redness, swelling) after the procedure.
What Recovery Really Looks Like?
Recovery typically involves limited weight-bearing, physical therapy, and regular follow-up visits. Most patients regain significant mobility and function within 3-6 months.
What Happens If You Delay Surgery?
Delaying hip replacement may result in increased pain, limited mobility, and potential joint damage. Early intervention can prevent further deterioration of the hip joint.
How to Prevent Recurrence or Failure?
Maintain a healthy weight, engage in low-impact exercises, and follow your physical therapist’s advice to optimize recovery and long-term hip function.
Nutrition and Bone or Joint Health
Ensure adequate intake of calcium and vitamin D to support bone health, and limit smoking and alcohol consumption for better healing outcomes.
Activity and Lifestyle Modifications
Post-surgery, engage in low-impact exercises such as swimming or cycling, and avoid activities that put excessive strain on the hip joint, such as heavy lifting or running.
Do you have more questions?
What are the main differences between anterior hip replacement and traditional posterior or lateral approaches?
The main difference lies in the surgical approach used to access the hip joint. Anterior hip replacement involves accessing the hip joint from the front, minimizing disruption to muscles and tendons. Traditional approaches, such as posterior or lateral, require dissection of these structures, potentially leading to longer recovery times.
How do I know if I’m a suitable candidate for anterior hip replacement surgery?
Suitable candidates typically have moderate to severe hip arthritis. Factors such as BMI and pelvic anatomy may influence candidacy. An evaluation by an orthopedic surgeon can determine eligibility based on individual circumstances.
Are there any specific risks or complications associated with anterior hip replacement compared to other techniques?
While anterior hip replacement offers advantages in terms of early recovery, there are potential risks such as nerve injury, fracture, and implant malposition. These risks are typically discussed during preoperative consultations.
How long does the procedure typically take, and what is the expected recovery time?
The duration of surgery varies but generally takes a couple of hours. Recovery time varies among patients but may involve immediate weight-bearing and discharge within a day or two. Full recovery can take several weeks to months.
What type of anesthesia is used for anterior hip replacement surgery?
General anesthesia is commonly used for anterior hip replacement, although regional anesthesia techniques may also be employed depending on the patient’s preferences and medical history.
Can you explain the process of muscle sparing in anterior hip replacement and how it contributes to quicker recovery?
Muscle sparing involves minimal disruption to muscles and tendons during surgery. This preservation of soft tissues allows for quicker recovery and reduced postoperative pain compared to traditional approaches.
Are there any specific preoperative preparations or precautions I should take before undergoing anterior hip replacement surgery?
Preoperative preparations may include medical evaluations, cessation of certain medications, and lifestyle modifications. Your surgeon will provide detailed instructions tailored to your individual needs.
What postoperative pain management options are available, and how effective are they?
Postoperative pain management may involve a combination of medications, regional anesthesia techniques, and physical therapy modalities. These approaches aim to minimize discomfort and facilitate recovery.
Will I need physical therapy after anterior hip replacement surgery, and if so, what does it entail?
Yes, physical therapy is typically recommended to improve strength, range of motion, and functional mobility. A physical therapist will create a personalized rehabilitation program focusing on these goals.
How soon after surgery can I expect to resume normal daily activities, such as walking and driving?
The timeline for resuming activities varies among patients but may begin shortly after surgery with guidance from your healthcare team. Driving restrictions may apply initially, depending on individual recovery progress.
Are there any restrictions on movement or weight-bearing following anterior hip replacement surgery?
Initially, precautions may be advised to protect the surgical site, such as avoiding excessive bending or twisting at the hip joint and adhering to weight-bearing instructions. Your surgeon will provide specific guidelines tailored to your surgery.
What are the potential benefits of anterior hip replacement surgery compared to other approaches in the long term?
Long-term benefits of anterior hip replacement include reduced risk of dislocation, faster recovery, and potentially improved functional outcomes. However, research on long-term outcomes is ongoing.
How frequently will I need follow-up appointments after surgery, and what will these involve?
Follow-up appointments are typically scheduled in the weeks and months following surgery to monitor healing, assess range of motion, and address any concerns. Your surgeon will determine the frequency based on your progress.
What measures are taken during surgery to minimize the risk of infection?
Sterile techniques, antibiotic prophylaxis, and meticulous wound care are employed to minimize the risk of infection during surgery. Additionally, surgical facilities adhere to strict protocols to maintain a sterile environment.
Are there any factors that could increase the likelihood of needing revision surgery in the future after anterior hip replacement?
Factors such as implant wear, instability, and osteolysis (bone loss) may increase the likelihood of needing revision surgery in the future. Regular follow-up appointments and adherence to postoperative instructions can help monitor and manage these risks.
Can you explain the role of X-rays during the procedure and in postoperative assessment?
X-rays are used intraoperatively to assess implant positioning and ensure accurate placement. Postoperatively, X-rays are utilized to evaluate implant stability, detect any abnormalities, and monitor healing progress.
How do you determine the appropriate size and positioning of the implant during surgery?
Surgical techniques, preoperative imaging, and intraoperative assessments are used to select the appropriate implant size and position based on the patient’s anatomy and specific surgical requirements.
What criteria do you use to assess the success of anterior hip replacement surgery?
Success is typically evaluated based on pain relief, functional improvement, implant stability, and patient satisfaction. Long-term outcomes, including implant survival rates, are also considered indicators of success.
Are there any lifestyle modifications or precautions I should take after surgery to prolong the longevity of the hip replacement?
Maintaining a healthy weight, engaging in regular low-impact exercise, and avoiding high-impact activities can help prolong the longevity of the hip replacement. Your surgeon may provide additional recommendations based on your individual circumstances.
What ongoing support or resources are available to patients undergoing anterior hip replacement surgery, both during recovery and in the long term?
Patients have access to various resources, including physical therapy services, educational materials, and support groups, to assist them during recovery and beyond. Your healthcare team can provide guidance on accessing these resources.

Dr. Sebastian Heaven
I provide Orthopaedic patient care at several different locations, including a Regional Joint Assessment Centre, a Level 1 Trauma Centre and a District General Hospital. My scope of practice is broad and includes Trauma, Arthroplasty and Sports Orthopaedics.
My areas of special interest include Primary and Revision Arthroplasty, Periprosthetic Fracture Management and general orthopaedic trauma management in isolation and in the context of complex polytrauma patients. I also have clinical research interests in these areas, as well the development of interprofessional relationships between trauma team members and fellow healthcare professionals.
I have personally written all or most of what's on this page for Complete Orthopedics, and approve the use of my content.
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
