Makoplasty Anterior Hip Replacement
MAKOplasty anterior hip replacement is a minimally invasive surgery that uses robotic assistance to replace the hip joint’s damaged parts. Unlike traditional hip replacement procedures, MAKOplasty provides a more precise alignment and positioning of the prosthetic components, leading to improved outcomes and faster recovery. By using the MAKO robotic system and the anterior approach, this technique minimizes soft tissue disruption, allowing for quicker post-surgical rehabilitation.
How Common It Is and Who Gets It? (Epidemiology)
MAKOplasty is primarily used for patients with hip arthritis, especially those who are younger and more active. Hip arthritis can result from osteoarthritis, inflammatory arthritis, or trauma. Although any age group can develop hip arthritis, MAKOplasty is particularly beneficial for younger patients with good bone quality who are in need of a hip replacement but want to preserve bone stock for potential future surgeries.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common cause of hip arthritis leading to hip replacement is osteoarthritis, where the cartilage that covers the ball and socket of the hip joint wears down over time, causing bone friction, pain, and limited movement. Other causes include post-traumatic arthritis due to injury or fractures and inflammatory arthritis conditions like rheumatoid arthritis.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint where the femoral head (ball) fits into the acetabulum (socket) of the pelvis. This joint is covered by smooth articular cartilage, which allows for frictionless movement. The hip joint allows the leg to move in various directions, crucial for daily activities like walking, running, and sitting.
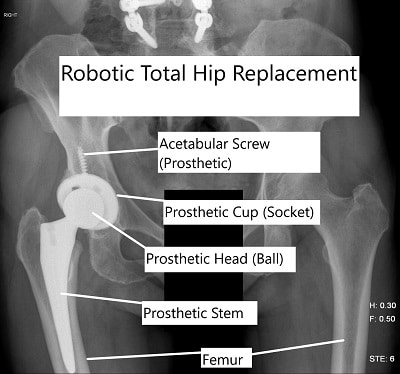
X-ray showing robotic total hip replacement
What You Might Feel – Symptoms (Clinical Presentation)
-
Pain: Persistent hip pain, especially when walking, bending, or standing up.
-
Stiffness: Limited range of motion, difficulty in bending or rotating the hip.
-
Decreased Mobility: Difficulty performing activities of daily living, such as walking or climbing stairs.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
X-rays: To check for joint space narrowing, bone spurs, and signs of arthritis.
-
MRI or CT scan: Provides detailed images of soft tissues and the bone structure for pre-surgical planning.
-
Physical exam: To assess the range of motion, muscle strength, and areas of pain.
Procedure Types or Techniques (Classification)
-
MAKOplasty: Robotic-assisted anterior hip replacement surgery.
-
Traditional Hip Replacement: Includes posterior or lateral approaches without robotic guidance.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Trochanteric bursitis: Inflammation of the bursa around the hip joint.
-
Sciatica: Pain radiating down the leg from the lower back.
-
Labral tears: A tear in the hip’s cartilage can cause similar pain and stiffness.
Treatment Options
-
Non-surgical: Medications (NSAIDs, pain relievers), physical therapy, injections, and lifestyle modifications (weight management, exercise).
-
Surgical: MAKOplasty anterior hip replacement, traditional total hip replacement, or hip resurfacing.
Recovery and What to Expect After Surgery
-
Initial Recovery: Patients often go home the same day or the next after surgery.
-
Physical Therapy: Begins immediately to improve strength and range of motion.
-
Full Recovery: Most patients can return to normal activities within 3-6 months, with minimal restrictions.
Possible Risks or Side Effects (Complications)
-
Infection: A risk with any surgery, though minimized with proper hygiene and surgical techniques.
-
Blood clots: Thrombosis or embolism, which can be prevented by early mobilization and blood thinners.
-
Dislocation: The risk of the prosthetic joint coming out of place, particularly in the initial recovery period.
-
Leg length discrepancy: A minor but possible outcome where one leg may be slightly longer or shorter than the other.
Long-Term Outlook (Prognosis)
-
Pain Relief: Significant reduction in pain and improved joint function is expected.
-
Implant Longevity: The implants typically last 15-20 years, depending on the patient’s age, activity level, and implant quality.
-
Functional Improvement: Most patients regain substantial mobility, with most able to resume daily activities and low-impact sports.
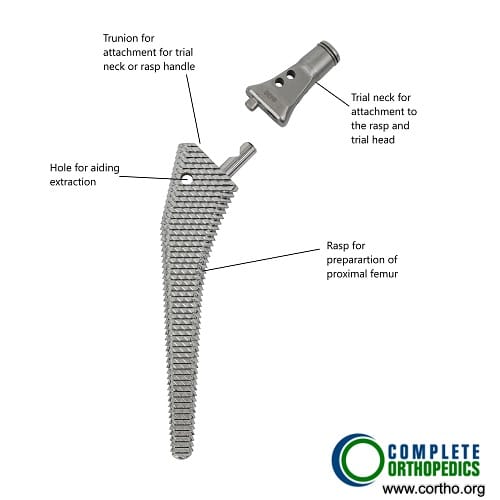
Rasp for preparing the femoral canal during hip replacement surgery
The images shows an instrument used in hip replacement surgery. The rasp has grooved surface to prepare the femoral canal to receive the prosthetic implant. The upper part has an attachment for handle to serially prepare the canal. once the final rasp is inserted for preparation, a trail head may be attached to the rasp to look for stability of the prosthetic implant.
Out-of-Pocket Cost
Medicare
CPT Code 27130 – Makoplasty Anterior Hip Replacement (Total Hip Arthroplasty via the Anterior Approach): $303.45
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans work alongside Medicare to fill the coverage gap and reduce financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which typically range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your Makoplasty anterior hip replacement is required due to a work-related injury or degenerative hip disease caused by your job, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip replacement surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Michael Johnson required a Makoplasty anterior hip replacement (CPT 27130) to treat hip arthritis. His estimated Medicare out-of-pocket cost was $303.45. Since Michael had supplemental insurance through AARP Medigap, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How long is the hospital stay?
A. Most patients stay for a short period, often going home the same day or the next day.
Q. How soon can I return to work?
A. Typically, patients can return to sedentary work within a few weeks and more physically demanding jobs in 2-3 months.
Q. Will I need physical therapy?
A. Yes, physical therapy is essential for recovery and begins almost immediately after surgery.
Summary and Takeaway
MAKOplasty anterior hip replacement is a state-of-the-art technique that offers precise implant placement using robotic guidance, reducing recovery time and post-operative pain. Ideal for younger, active patients, it provides lasting pain relief and improved function with fewer complications compared to traditional approaches.
Clinical Insight & Recent Findings
A recent study investigated the impact of robotic-assisted MAKOplasty anterior hip replacement on blood loss compared to conventional methods. The study found no significant difference in postoperative hemoglobin levels or the need for blood transfusions between the robotic-assisted and conventional surgery groups.
Although MAKOplasty is associated with reduced soft tissue disruption and improved alignment, these advantages did not translate into a statistically significant reduction in blood loss in this cohort.
This aligns with the general trend observed in robotic-assisted surgeries, where benefits are noted in other metrics like recovery time but may not substantially affect bleeding outcomes. (“Study on MAKOplasty and blood loss – see PubMed”).
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in joint replacement surgery perform the procedure, with assistance from robotic technology specialists and surgical teams.
When to See a Specialist?
If you are experiencing chronic hip pain that limits your daily activities and have not found relief from conservative treatments, consult an orthopedic surgeon to discuss surgical options.
When to Go to the Emergency Room?
Seek emergency medical help if you experience sudden, severe pain, or signs of infection, such as fever, redness, or swelling at the surgical site.
What Recovery Really Looks Like?
Recovery involves pain management, physical therapy, and follow-up visits. Most patients regain significant function within 3-6 months, with gradual improvement over time.
What Happens If You Delay Surgery?
Delaying surgery can lead to worsening pain, further joint damage, and potentially a more complicated procedure if surgery is postponed for too long.
How to Prevent Recurrence or Failure?
To ensure the longevity of your implant, maintain a healthy weight, avoid high-impact activities, and follow post-surgery instructions regarding physical therapy and activity restrictions.
Nutrition and Bone or Joint Health
Ensure adequate intake of calcium and vitamin D to support bone health. Avoid smoking and limit alcohol consumption to optimize recovery and implant longevity.
Activity and Lifestyle Modifications
After surgery, engage in low-impact activities such as swimming or cycling. Avoid heavy lifting and high-impact activities to protect the implant.
Do you have more questions?
How does the recovery time for MakoPlasty compare to other minimally invasive hip replacement techniques?
Recovery time for MakoPlasty is often shorter compared to traditional hip replacement surgeries due to its minimally invasive nature and precision.
Are there any specific age limitations for patients undergoing MakoPlasty Anterior Hip Replacement?
Age alone isn’t a determining factor. The candidacy depends more on overall health and bone quality.
What are the potential complications associated with the robotic components used in MakoPlasty surgery?
Potential complications are minimal and may include injury to surrounding structures, although such occurrences are rare due to the precision of the robotic system.
Can MakoPlasty technology be used to correct leg length inequality after hip replacement surgery?
Yes, MakoPlasty can address leg length discrepancies by precisely adjusting implant placement during surgery.
Are there any specific exercises or rehabilitation protocols recommended after MakoPlasty surgery?
Yes, rehabilitation typically involves physical therapy exercises to improve strength, flexibility, and mobility, tailored to each patient’s needs.
How long does the MakoPlasty procedure typically take from start to finish?
The duration varies but generally takes around 1-2 hours, depending on factors such as patient anatomy and complexity of the case.
What factors determine whether a patient is a good candidate for MakoPlasty versus traditional hip replacement?
Factors include age, bone quality, overall health, and surgeon preference. MakoPlasty is particularly beneficial for patients with complex anatomies or those seeking a more precise outcome.
Are there any dietary restrictions or nutritional recommendations before and after MakoPlasty surgery?
Generally, no specific dietary restrictions are necessary, but maintaining a balanced diet rich in nutrients can aid in recovery.
Can MakoPlasty Anterior Hip Replacement be performed on patients with a history of prior hip surgeries?
Yes, MakoPlasty can be performed on patients with a history of prior hip surgeries, although individual circumstances may vary.
How does the cost of MakoPlasty surgery compare to traditional hip replacement methods?
The cost may vary depending on factors such as hospital fees, surgeon fees, and insurance coverage. In some cases, MakoPlasty may be slightly more expensive due to the advanced technology involved. However, long-term benefits may outweigh the initial costs.
What is the long-term success rate of MakoPlasty Anterior Hip Replacement compared to traditional methods?
Long-term success rates are generally favorable for MakoPlasty, with many patients experiencing improved function and pain relief. However, individual outcomes may vary.
Can MakoPlasty technology be used for other types of joint replacement surgeries besides the hip?
Yes, MakoPlasty technology is also used for knee replacement surgeries, providing similar benefits of precision and minimal invasiveness.
What are the potential risks associated with anesthesia during MakoPlasty surgery?
Anesthesia risks are similar to those of any surgical procedure and may include reactions to medications, respiratory issues, or complications related to pre-existing medical conditions. However, these risks are typically low and managed by experienced anesthesia providers.
Is MakoPlasty suitable for patients with severe hip arthritis or advanced joint degeneration?
MakoPlasty may still be an option for some patients with advanced arthritis or joint degeneration, especially if they have complex anatomies that require precise implant placement.
How soon after MakoPlasty surgery can patients return to driving and other daily activities?
Patients typically resume driving and light daily activities within a few weeks to a month after surgery, depending on individual recovery progress and clearance from their surgeon.
Are there any restrictions on bending, twisting, or lifting heavy objects after MakoPlasty surgery?
Initially, patients are advised to avoid strenuous activities and heavy lifting to allow for proper healing. Specific restrictions may vary depending on individual circumstances and surgeon recommendations.
Can MakoPlasty surgery be performed on both hips simultaneously?
While it is possible to perform bilateral MakoPlasty surgeries, this approach may increase the complexity of recovery and rehabilitation and is typically reserved for select cases.
What measures are taken to ensure proper alignment and stability of the hip joint during MakoPlasty surgery?
The robotic arm system used in MakoPlasty provides real-time feedback to the surgeon, enabling precise adjustments to optimize implant placement and joint alignment.
Is there a risk of infection or implant-related complications after MakoPlasty surgery?
While all surgeries carry some risk of infection or implant-related issues, MakoPlasty’s minimally invasive approach and sterile techniques help minimize these risks.
How does MakoPlasty technology accommodate for variations in patient anatomy and hip joint structure?
MakoPlasty utilizes advanced imaging and 3D mapping techniques to create personalized surgical plans tailored to each patient’s unique anatomy, ensuring optimal outcomes.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
