Minimally Invasive Total Hip Replacement
Minimally invasive total hip replacement (THR) is a modern surgical technique used to replace the hip joint, involving smaller incisions and less disruption to surrounding muscles compared to traditional methods. This approach has gained popularity due to its potential for quicker recovery, less postoperative pain, and smaller scars. While it offers several benefits, it may not be suitable for all patients, particularly those with complex or pre-existing hip conditions.
How Common It Is and Who Gets It? (Epidemiology)
Minimally invasive hip replacement is typically recommended for individuals with hip arthritis that has not responded to conservative treatments. It is most beneficial for patients who are in generally good health, have low-to-normal body mass index (BMI), and do not have significant muscle mass or hip deformities that could complicate the surgery.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common reason for hip replacement surgery is osteoarthritis, a condition where the cartilage of the hip joint wears away, leading to pain, stiffness, and reduced mobility. Other conditions such as rheumatoid arthritis, trauma, or hip dysplasia can also lead to the need for hip replacement.
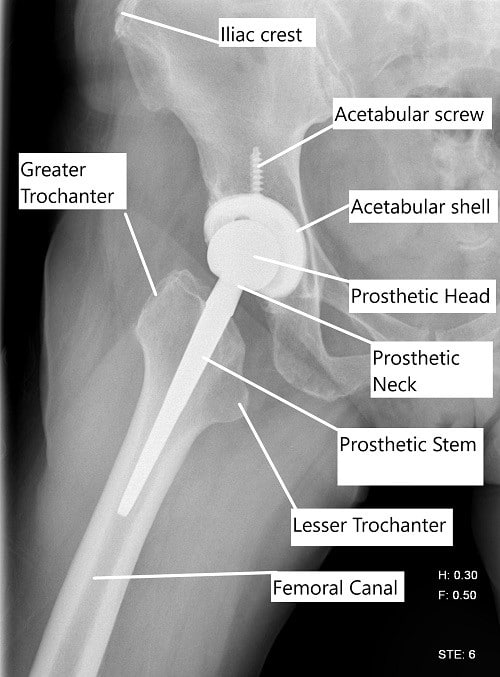
X-ray showing a lateral view of a total hip replacement.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint, with the femoral head (ball) fitting into the acetabulum (socket) of the pelvis. The smooth cartilage that covers the ball and socket allows for frictionless movement, enabling a wide range of motion necessary for walking, running, and sitting.
What You Might Feel – Symptoms (Clinical Presentation)
-
Pain: Persistent pain in the hip, particularly when walking, bending, or standing.
-
Stiffness: Limited range of motion, difficulty moving the hip in all directions.
-
Difficulty Walking: Limping or inability to bear weight due to joint pain.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
X-rays: To examine the joint space, bone deformities, and arthritis.
-
MRI or CT scans: To visualize soft tissues and detailed bone structures.
-
Physical Exam: To assess the range of motion and identify pain points.
Procedure Types or Techniques (Classification)
-
Traditional THR: Larger incision, more muscle disruption.
-
Minimally Invasive THR: Smaller incision, reduced muscle disruption, quicker recovery.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Trochanteric bursitis: Inflammation of the bursa near the hip joint.
-
Sciatica: Pain that radiates down the leg due to nerve compression.
-
Labral tears: Damage to the cartilage in the hip joint, causing similar symptoms.
Treatment Options
Non-surgical: Pain medications (NSAIDs, acetaminophen), physical therapy, corticosteroid injections, and assistive devices like canes.
Surgical: Minimally invasive THR, traditional THR, or hip resurfacing.
Recovery and What to Expect After Surgery
-
Immediate Post-Surgery: Patients can bear weight on the leg soon after surgery, typically with the aid of crutches.
-
Physical Therapy: Begins early to restore motion and strength.
-
Full Recovery: Most patients regain full functionality within 3-6 months, with some returning to activities like walking, swimming, or biking.
Possible Risks or Side Effects (Complications)
-
Infection: A risk with any surgical procedure.
-
Blood Clots: Can form in the legs, with potential for a pulmonary embolism.
-
Dislocation: Rare but possible during the initial recovery period.
-
Leg Length Discrepancy: Slight difference in leg length after surgery.
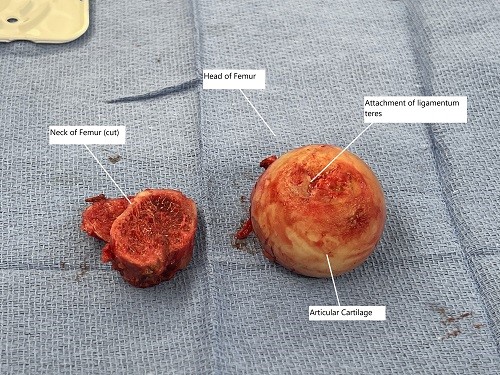
Intraoperative image showing the removed head of the femur and the neck of the femur.
Long-Term Outlook (Prognosis)
-
Pain Relief: Most patients experience significant pain relief and improved joint function.
-
Implant Longevity: Implants typically last 15-20 years, depending on activity level and patient factors.
-
Functional Improvement: Most patients regain substantial mobility and independence.
Out-of-Pocket Cost
Medicare
CPT Code 27130 – Minimally Invasive Total Hip Replacement (Total Hip Arthroplasty with a Smaller Incision): $303.45
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans work alongside Medicare to fill the coverage gap and reduce patient financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which typically range between $100 and $300, depending on your plan and provider network.
Workers’ Compensation
If your minimally invasive total hip replacement is required due to a work-related injury or degenerative hip disease caused by your job, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip replacement surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Sarah Lee required minimally invasive total hip replacement (CPT 27130) to treat advanced osteoarthritis in her hip. Her estimated Medicare out-of-pocket cost was $303.45. Since Sarah had supplemental insurance through Blue Cross Blue Shield, her remaining balance was fully covered, leaving her with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. How long is the hospital stay?
A. Typically, patients go home the same day or the next after surgery.
Q. When can I return to work?
A. For sedentary jobs, patients can return in 2-4 weeks; for more physically demanding work, it may take 6-8 weeks.
Q. What activities can I do after surgery?
A. Low-impact activities like swimming, walking, and cycling are encouraged; high-impact sports should be avoided for the long term.
Summary and Takeaway
Minimally invasive total hip replacement is an effective option for patients with hip arthritis who want to restore function and reduce pain. This technique offers benefits like faster recovery, less tissue damage, and smaller scars compared to traditional hip replacement. However, it may not be suitable for all patients, and a thorough consultation with an orthopedic surgeon is essential to determine the best approach.
Clinical Insight & Recent Findings
A recent study evaluated the early clinical and radiological outcomes of minimally invasive total hip replacement (MI THR) using the posterolateral approach.
The study found that the procedure, performed on 73 hips, yielded significant improvements in the Harris Hip Scores (HHS) and demonstrated favorable acetabular component positioning in the majority of cases. While blood loss was lower than expected, there were some complications, including a nondisplaced femoral fracture and early dislocation due to malpositioned components.
Overall, the minimally invasive technique provided satisfactory results with a lower complication rate compared to traditional approaches. (“Study on minimally invasive total hip replacement – see PubMed”).
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in joint replacement surgery perform the procedure, assisted by a surgical team and possibly robotic technology specialists.
When to See a Specialist?
If you have persistent hip pain that limits your daily activities and have not found relief from conservative treatments, consult an orthopedic surgeon to discuss surgical options.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience severe pain, signs of infection (fever, redness, swelling), or if the joint dislocates.
What Recovery Really Looks Like?
Recovery includes pain management, physical therapy, and gradual return to normal activities. Most patients regain significant function within 3-6 months, with minimal restrictions.
What Happens If You Delay Surgery?
Delaying surgery can lead to worsening pain, further joint deterioration, and potentially more complex surgery.
How to Prevent Recurrence or Failure?
Maintain a healthy weight, avoid high-impact activities, and follow post-surgery rehabilitation plans to ensure the longevity of your implant.
Nutrition and Bone or Joint Health
Ensure adequate intake of calcium and vitamin D for bone health. Avoid smoking and limit alcohol consumption to support recovery and implant durability.
Activity and Lifestyle Modifications
Post-surgery, engage in low-impact activities and avoid heavy lifting and high-impact sports to protect the implant and promote recovery.
Do you have more questions?
What is the typical recovery time for patients undergoing minimally invasive total hip replacement surgery?
Recovery time can vary depending on individual factors, but many patients are able to return to normal activities within a few weeks to months after surgery.
Are there any specific post-operative rehabilitation exercises recommended for patients undergoing minimally invasive total hip replacement?
patients typically undergo physical therapy to improve strength, flexibility, and range of motion in the hip joint following surgery.
How does minimally invasive total hip replacement differ from traditional hip replacement surgery?
Minimally invasive techniques involve smaller incisions and less disruption to surrounding tissues, potentially leading to shorter hospital stays, faster recovery, and less post-operative pain compared to traditional surgery.
What are the potential risks and complications associated with minimally invasive total hip replacement?
While complications are rare, they can include infection, blood clots, implant loosening, nerve injury, or fracture. Your surgeon will discuss these risks and how they are minimized during the procedur
Can minimally invasive total hip replacement be performed on patients with severe hip arthritis or other underlying conditions?
Yes, in many cases, minimally invasive surgery is suitable for patients with severe hip arthritis or other conditions affecting the hip joint.
How is the accuracy of implant placement ensured during minimally invasive total hip replacement?
Advanced imaging techniques and robotic-assisted technology may be used to ensure precise implant placement and optimal alignment of the hip joint.
What type of anesthesia is typically used for minimally invasive total hip replacement surgery?
Patients may receive either general anesthesia or regional anesthesia, depending on their medical history and the preference of the surgical team.
How soon after surgery can patients expect to experience pain relief and improved mobility?
Many patients experience significant pain relief and improved mobility shortly after surgery, with continued improvement over the following weeks and months.
Are there any specific lifestyle modifications or precautions recommended for patients following minimally invasive total hip replacement?
Patients may be advised to avoid high-impact activities and certain movements that could put excessive stress on the hip joint. Your surgeon will provide guidance based on your individual circumstances.
What factors determine whether a patient is a suitable candidate for minimally invasive total hip replacement?
Factors such as the severity of hip arthritis, overall health, bone quality, and lifestyle goals are considered when determining candidacy for surgery.
How long do the benefits of minimally invasive total hip replacement typically last?
The benefits of surgery can be long-lasting, providing patients with improved function and pain relief for many years. However, individual results may vary.
What pre-operative preparations are necessary for patients undergoing minimally invasive total hip replacement?
Pre-operative preparations may include medical evaluations, imaging tests, cessation of certain medications, and lifestyle modifications to optimize surgical outcomes.
Are there any dietary restrictions or nutritional guidelines that patients should follow before or after surgery?
While there are no specific dietary restrictions, maintaining a balanced diet rich in nutrients can support the healing process and overall recovery.
How is post-operative pain managed for patients undergoing minimally invasive total hip replacement?
Pain management techniques may include a combination of oral medications, regional anesthesia, nerve blocks, or other modalities to ensure patient comfort during recovery.
What are the potential benefits of minimally invasive total hip replacement compared to traditional surgery?
Potential benefits include smaller incisions, reduced tissue damage, faster recovery, shorter hospital stays, and less post-operative pain.
Can minimally invasive total hip replacement be performed as an outpatient procedure?
In some cases, minimally invasive surgery may be performed on an outpatient basis, allowing patients to return home on the same day as surgery.
What follow-up care is necessary after minimally invasive total hip replacement surgery?
Follow-up care typically involves regular post-operative appointments with your surgeon to monitor healing, address any concerns, and track your progress.
How soon can patients resume driving and other normal activities after minimally invasive total hip replacement?
Patients may be able to resume driving and light activities within a few weeks after surgery, with more strenuous activities gradually introduced as healing progresses.
Are there any age restrictions for patients undergoing minimally invasive total hip replacement?
Age alone is not a determining factor for candidacy, as suitability for surgery depends on overall health and individual circumstances.
Can minimally invasive total hip replacement be performed using robotic-assisted technology?
Yes, robotic-assisted technology may be used to enhance precision and accuracy during minimally invasive hip replacement surgery.
How is infection risk minimized during minimally invasive total hip replacement surgery?
Strict adherence to sterile techniques, antibiotic prophylaxis, and other infection prevention protocols are utilized to minimize the risk of surgical site infections.
Are there any long-term complications associated with minimally invasive total hip replacement?
While complications are rare, long-term issues such as implant wear, loosening, or dislocation may occur in some patients, necessitating further evaluation and management.
What is the success rate of minimally invasive total hip replacement surgery?
Minimally invasive hip replacement surgery has generally high success rates, with many patients experiencing significant improvement in pain and function following the procedure.
How soon can patients expect to return to work or other regular activities after minimally invasive total hip replacement surgery?
Return to work and other regular activities can vary depending on individual factors such as job requirements, overall health, and the type of activities involved. However, many patients are able to resume normal activities within a few weeks to months after surgery.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
