Posterior Hip Replacement
Posterior hip replacement is one of the most commonly performed surgical procedures for patients suffering from severe hip arthritis. This approach, also known as Moore’s or the Southern approach, provides a thorough exposure of the hip joint without cutting through key muscle groups involved in normal walking. The procedure involves replacing the damaged or arthritic parts of the hip with prosthetic components to restore joint function and alleviate pain.
How Common It Is and Who Gets It? (Epidemiology)
Hip arthritis, often due to osteoarthritis, is the primary reason for hip replacement surgery. This condition causes pain, stiffness, and decreased mobility, leading many patients, particularly elderly individuals, to consider surgical intervention. Posterior hip replacement is typically recommended when nonsurgical methods like medications, physical therapy, or injections no longer provide adequate relief.
Why It Happens – Causes (Etiology and Pathophysiology)
-
Osteoarthritis: The most common cause of hip arthritis, characterized by the wearing down of cartilage.
-
Rheumatoid Arthritis: An autoimmune condition causing joint inflammation and degeneration.
-
Hip Dysplasia: A condition where the acetabulum (hip socket) doesn’t form properly, leading to joint instability and wear.
-
Avascular Necrosis: A condition where the blood supply to the femoral head is disrupted, leading to bone death.
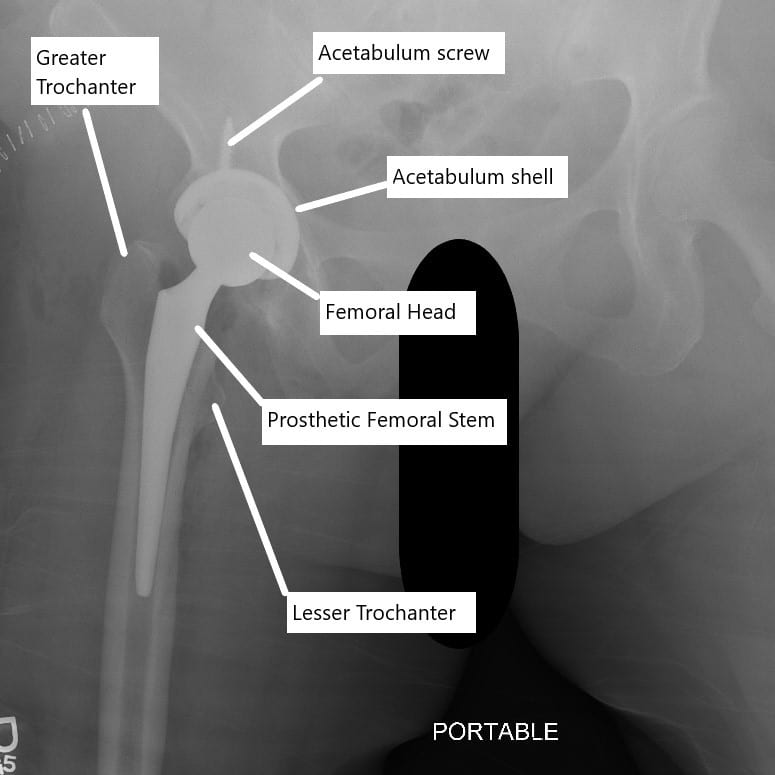
X-ray showing total hip replacement.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint consisting of the femoral head (ball) and the acetabulum (socket) in the pelvis. The articular cartilage covering these structures allows for smooth movement. When the cartilage wears down, typically due to arthritis, the bones begin to rub together, causing pain and stiffness.
What You Might Feel – Symptoms (Clinical Presentation)
-
Pain: Often in the groin or thigh, particularly when moving or bearing weight.
-
Stiffness: Difficulty moving the hip, especially with bending or rotating the leg.
-
Decreased Mobility: Limited ability to walk, climb stairs, or perform daily tasks.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
X-rays: To examine joint space narrowing and changes in bone structure.
-
MRI or CT scan: Used to assess soft tissues and detect other issues like labral tears.
-
Physical Exam: To assess range of motion and pain levels.
Procedure Types or Techniques (Classification)
-
Posterior Approach: The most common method, involving an incision at the back of the hip.
-
Anterior Approach: Accessing the joint from the front, offering benefits like quicker recovery.
-
Lateral and Anterolateral Approaches: Less commonly used, involving incisions at the side of the hip.

Intraoperative image showing posterior hip replacement.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Trochanteric Bursitis: Inflammation of the bursa near the hip.
-
Sciatica: Nerve pain that radiates from the lower back to the hip and leg.
-
Labral Tears: Tears in the cartilage around the hip socket.
Treatment Options
-
Non-surgical: Medications, physical therapy, injections, and lifestyle modifications.
-
Surgical: Posterior hip replacement or other surgical approaches, depending on the patient’s condition and anatomy.
Recovery and What to Expect After Surgery
-
Immediate Post-op: Patients may start walking with assistance on the day following surgery, with weight-bearing supported by crutches.
-
Physical Therapy: Begins shortly after surgery to restore mobility and strengthen the hip.
-
Full Recovery: Most patients regain substantial function and independence within 6-12 weeks.
Possible Risks or Side Effects (Complications)
-
Infection: A risk with any surgical procedure.
-
Blood Clots: Deep vein thrombosis (DVT) can occur.
-
Dislocation: The hip implant may dislocate if not properly positioned.
-
Leg Length Discrepancy: A slight difference in leg length post-surgery.
-
Fracture: Rare, but possible during or after surgery.
Long-Term Outlook (Prognosis)
-
Success: Most patients experience significant pain relief and regain mobility after posterior hip replacement. The prosthetic hip joint typically lasts 15-20 years or more.
-
Ongoing Care: Patients are advised to avoid high-impact activities to prolong the lifespan of the implant.
Out-of-Pocket Cost
Medicare
CPT Code 27130 – Posterior Hip Replacement (Total Hip Arthroplasty via the Posterior Approach): $303.45
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans work alongside Medicare to fill the coverage gap and reduce patient financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which typically range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your posterior hip replacement is required due to a work-related injury or degenerative hip disease caused by your job, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip replacement surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
John Smith underwent posterior hip replacement (CPT 27130) due to severe hip arthritis. His estimated Medicare out-of-pocket cost was $303.45. Since John had supplemental insurance through Blue Cross Blue Shield, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. What is the recovery time for posterior hip replacement?
A. Recovery typically takes 6-12 weeks, with most patients returning to normal activities within 3 months.
Q. Can I drive after hip replacement?
A. Most patients can drive within 4-6 weeks, depending on the leg and recovery process.
Q. How long do hip implants last?
A. Hip implants typically last 15-20 years, though this may vary depending on activity level and other factors.
Summary and Takeaway
Posterior hip replacement is a proven and highly successful procedure for patients with hip arthritis or severe joint damage. It offers significant pain relief and functional improvement, although the recovery time can vary. The posterior approach remains the gold standard in hip replacement surgeries due to its reliable outcomes and good access to the hip joint.
Clinical Insight & Recent Findings
A recent study compared the direct anterior approach (DAA) and the posterolateral approach (PLA) for total hip replacement in middle-aged and elderly patients with femoral neck fractures. Researchers found that the anterior approach led to shorter surgery times, smaller incisions, less blood loss, and faster postoperative recovery than the posterior method.
Patients who underwent the DAA also reported lower pain levels and higher hip function scores in the first six months after surgery, though outcomes were similar at one year. Importantly, complication rates and implant alignment were comparable between the two approaches.
Overall, the study concludes that the anterior approach offers clear short-term advantages in recovery speed and reduced surgical trauma, supporting its broader use in clinical practice. (“Study comparing anterior vs. posterior hip replacement outcomes – see PubMed.“)
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in joint replacement perform posterior hip replacement surgeries, assisted by anesthesiologists, surgical nurses, and physical therapists.
When to See a Specialist?
If you experience persistent hip pain that affects your daily activities and non-surgical treatments have not helped, it may be time to consult an orthopedic surgeon.
When to Go to the Emergency Room?
Seek immediate medical attention if you experience signs of infection (fever, redness, swelling), a hip dislocation, or severe pain after surgery.
What Recovery Really Looks Like?
Recovery typically involves managing pain, following a physical therapy regimen, and gradually returning to normal activities. Most patients regain significant function within 6-12 weeks, with minimal restrictions.
What Happens If You Delay Surgery?
Delaying surgery may result in further joint deterioration, increased pain, and more complex surgery later on.
How to Prevent Recurrence or Failure?
Follow your surgeon’s recommendations, maintain a healthy weight, and avoid high-impact activities to ensure the longevity of the hip implant.
Nutrition and Bone or Joint Health
Ensure adequate intake of calcium and vitamin D to support bone health and prevent future complications.
Activity and Lifestyle Modifications
Engage in low-impact activities and follow your surgeon’s guidelines for long-term care and mobility.
Do you have more questions?
How does a PCL injury affect knee stability?
A PCL injury can significantly compromise knee stability, as the ligament plays a critical role in controlling the backward movement of the tibia under the femur.
How does posterior hip replacement differ from other approaches?
Unlike anterior or lateral approaches, posterior hip replacement involves accessing the hip joint through the back of the hip, allowing for exposure and placement of the prosthetic components.
What types of hip conditions or injuries are commonly treated with posterior hip replacement?
Posterior hip replacement is often used to treat conditions such as osteoarthritis, rheumatoid arthritis, avascular necrosis, hip fractures, and other degenerative hip disorders.
How is posterior hip replacement surgery performed?
During posterior hip replacement surgery, an incision is made at the back of the hip, and the damaged portions of the hip joint are removed and replaced with prosthetic components, including a metal stem inserted into the femur, a metal or ceramic ball attached to the stem, and a socket implanted in the acetabulum.
What are the benefits of posterior hip replacement?
Posterior hip replacement offers advantages such as excellent exposure of the hip joint, familiar surgical technique for many orthopedic surgeons, and good long-term outcomes in terms of pain relief and improved function.
What are the potential risks or complications associated with posterior hip replacement?
Risks and complications of posterior hip replacement may include infection, blood clots, dislocation of the prosthetic hip joint, nerve or blood vessel injury, leg length inequality, implant loosening, and the need for revision surgery.
How does the recovery process differ for posterior hip replacement compared to other approaches?
Recovery after posterior hip replacement may involve specific precautions to prevent hip dislocation, such as avoiding certain movements and positions during the initial healing phase. Physical therapy and rehabilitation are also essential components of the recovery process.
What factors determine whether a patient is a suitable candidate for posterior hip replacement?
Patient factors such as overall health, age, bone quality, hip joint anatomy, and the presence of any pre-existing medical conditions influence the decision to undergo posterior hip replacement surgery.
Are there any restrictions on physical activities or movements after posterior hip replacement surgery?
Patients may need to avoid certain movements and activities that place excessive stress on the hip joint, especially during the early stages of recovery. However, most individuals can gradually resume normal activities as tolerated with guidance from their healthcare provider.
How long does it take to fully recover from posterior hip replacement surgery?
The timeline for full recovery after posterior hip replacement varies depending on factors such as the patient’s age, overall health, adherence to post-operative instructions, and the extent of hip joint damage. However, many patients experience significant improvement within several weeks to months after surgery.
What are the potential long-term outcomes of posterior hip replacement?
Long-term outcomes of posterior hip replacement surgery may include pain relief, improved hip function, increased mobility, and enhanced quality of life for many patients. However, individual results may vary depending on factors such as patient age, activity level, and overall health.
What is the typical lifespan of prosthetic components used in posterior hip replacement?
The lifespan of prosthetic components used in posterior hip replacement varies depending on factors such as patient age, activity level, implant type, and implant material. In general, modern prosthetic components are designed to last 15-20 years or more with proper care and regular follow-up.
How does the risk of nerve injury differ between posterior hip replacement and other approaches?
Posterior hip replacement carries a risk of injury to the sciatic nerve, which runs close to the surgical site. However, advances in surgical technique and intraoperative monitoring have reduced the incidence of nerve injury in recent years.
What are the factors that influence the choice between posterior hip replacement and other surgical approaches?
Factors such as surgeon expertise, patient anatomy, hip joint pathology, patient preferences, and the presence of any pre-existing conditions or surgical risk factors influence the choice of surgical approach for hip replacement.
How does the risk of blood loss differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of blood loss compared to anterior or lateral approaches due to the larger incision and potential disruption of more soft tissue structures. However, transfusion rates are typically low with modern surgical techniques and blood conservation strategies.
Can posterior hip replacement be performed in patients with pre-existing medical conditions?
Posterior hip replacement may be performed in patients with certain pre-existing medical conditions, depending on the severity and stability of the conditions and the overall surgical risk. However, careful pre-operative evaluation and optimization may be necessary to minimize the risk of complications.
How does the risk of implant loosening differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of implant loosening compared to anterior or lateral approaches, particularly in patients with poor bone quality or suboptimal implant positioning. However, advances in implant design and surgical technique have improved implant stability and longevity in recent years.
Are there any specific post-operative precautions or instructions for patients undergoing posterior hip replacement?
Yes, patients undergoing posterior hip replacement surgery may receive specific post-operative precautions to minimize the risk of hip dislocation, such as avoiding crossing the legs, bending the hip beyond a certain angle, or sitting on low chairs or sofas. Compliance with these precautions is essential for successful recovery.
How does the risk of leg length inequality differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of leg length inequality compared to other approaches, as precise restoration of leg length and alignment may be more challenging due to the posterior surgical approach. However, careful pre-operative planning and intraoperative techniques can help minimize this risk.
Can posterior hip replacement be performed using robotic-assisted techniques?
Yes, posterior hip replacement surgery can be performed using robotic-assisted techniques, which offer potential benefits such as improved accuracy in implant placement, enhanced surgical precision, and better patient outcomes. Robotic technology may be particularly useful in cases involving complex hip anatomy or revision surgery.
How does the risk of infection differ between posterior hip replacement and other approaches?
Posterior hip replacement carries a risk of surgical site infection similar to other surgical approaches, although infection rates are typically low with modern surgical techniques and perioperative antibiotic prophylaxis. However, patient-specific factors such as immunocompromised status or obesity may increase the risk of infection in some cases.
Can posterior hip replacement be performed in patients with previous hip surgeries or revisions?
Yes, posterior hip replacement surgery can be performed in patients with a history of previous hip surgeries or revisions, depending on the specific circumstances and the underlying hip pathology. However, careful pre-operative evaluation and surgical planning are essential to address any anatomical challenges or complications from prior surgeries.
How does the risk of perioperative complications differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of certain perioperative complications such as nerve injury, wound healing problems, and blood loss compared to other approaches. However, careful patient selection, meticulous surgical technique, and adherence to evidence-based practices can help minimize the risk of complications in all approaches.
Are there any specific intraoperative considerations or techniques used in posterior hip replacement surgery?
Yes, posterior hip replacement surgery requires careful soft tissue dissection and retraction to access the hip joint from the back. Intraoperative techniques such as capsular repair, femoral head osteotomy, and acetabular reaming may be used to optimize implant placement and stability.
How does the risk of dislocation differ between posterior hip replacement and other approaches?
Posterior hip replacement may be associated with a slightly higher risk of hip dislocation compared to anterior or lateral approaches due to the posterior soft tissue structures being disrupted during surgery. However, careful surgical technique, appropriate implant selection, and patient education can help minimize this risk.
Can posterior hip replacement be performed using tissue-sparing approaches such as muscle-sparing techniques?
Yes, posterior hip replacement surgery can be performed using tissue-sparing techniques, which aim to minimize soft tissue damage, reduce post-operative pain, and accelerate recovery. These techniques typically involve smaller incisions and less disruption to surrounding muscles and tendons.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
