Revision Hip Replacement
Revision hip replacement is a surgical procedure performed to replace the components of a previously implanted total hip replacement (THR). It is typically required when the original hip replacement components fail due to various reasons such as wear and tear, loosening, infection, or trauma. The goal of revision hip replacement, like primary hip replacement, is to alleviate pain and restore mobility, allowing patients to return to their normal activities.
How Common It Is and Who Gets It? (Epidemiology)
While total hip replacement is a highly successful procedure, revision hip replacement is less common. However, it becomes necessary in a small subset of patients, particularly those who have had their initial hip replacement for 10-20 years. Younger, more active patients with longer life expectancy are at higher risk of implant failure and may need revision surgery sooner. Hip revision surgeries are becoming more common as the number of patients receiving hip replacements increases.
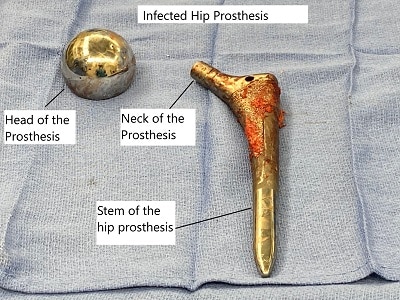
Prosthetic components removed due to failure.
Components of Total Hip Replacement
- Acetabulum cup made of metal alloy or ceramic. It is is fixed with screws or press-fitted in the socket forming the Hip joint after removing damaged
- A special form of highly durable plastic called polyethylene is placed in the socket to allow smooth gliding
- A stem made of metallic alloy is inserted in the upper part of the thigh bone (femur). The stem may be press-fit or fixed using a special form of bone cement.
- A prosthetic head made of metal alloy or ceramic is placed on the stem replacing the natural head of the femur.

Acetabular shell with multiple screw hole options.
The acetabular shell is usually press fitted in the acetabular cavity. The acetabular cavity is prepared by reaming the cavity that allows new bone to grow into the outer porous coating of the acetabular shell. The multiple screw options are advantageous in revision surgery.
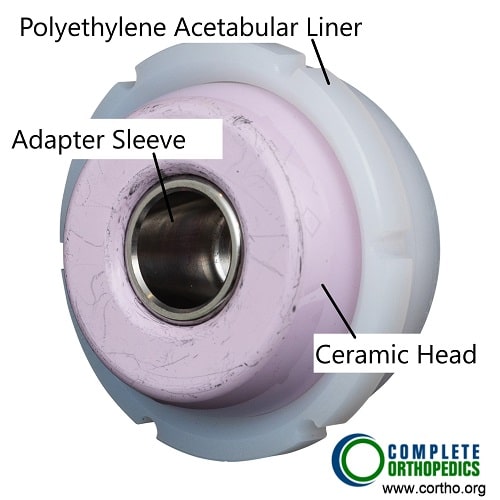
Prosthetic femoral head and acetabular liner
The acetabular liner made of highly cross linked polyethylene fits in the acetabular shell and provides a smooth surface for the prosthetic head to rotate in the cavity. The prosthetic head may be made of ceramic or cobalt chromium alloy.
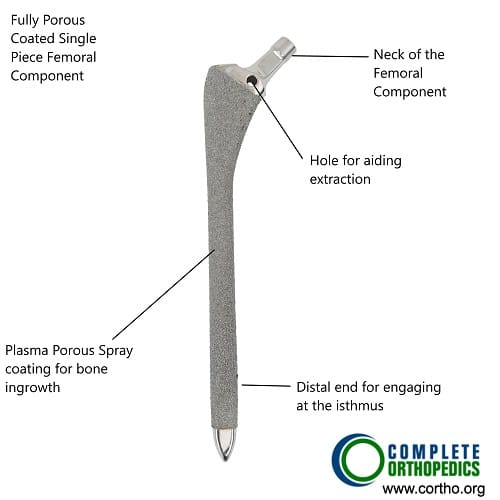
Fully porous coated long femoral stem with anatomical bow.
During revision surgery, a fully porous coated femoral stem is usually used for a better stability of the component. The stem is also longer than the primary prosthesis to provide more stability. Other types of stems may be used that may have detachable upper and lower parts (modular stems).
Why It Happens – Causes (Etiology and Pathophysiology)
The failure of hip replacement components can occur due to:
-
Wear and Tear: The prosthetic components, particularly the polyethylene liner, can wear down over time, leading to loosening of the implant.
-
Loosening of the Implant: This can be caused by improper fixation of the prosthesis to the bone or the breakdown of bone cement.
-
Infection: Bacteria can enter the surgical site and cause infection, leading to implant loosening.
-
Trauma: Accidents or falls can cause fractures around the implant or dislocations, requiring revision surgery.
-
Dislocation: Improper alignment of the prosthetic components can lead to recurrent dislocations, necessitating revision.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint consisting of the femoral head (ball) and the acetabulum (socket) in the pelvis. The femoral head is covered by a smooth cartilage layer that allows for frictionless movement within the socket. In a healthy hip, the joint allows for a wide range of motion necessary for activities such as walking, running, and sitting. When arthritis or injury damages the cartilage and bone, hip replacement surgery may be required.
What You Might Feel – Symptoms (Clinical Presentation)
-
Pain: Recurring or persistent pain in the hip joint, especially after physical activity or weight-bearing.
-
Stiffness: Difficulty moving the hip joint or performing everyday tasks such as walking or bending.
-
Instability: A feeling that the hip may give way or dislocate.
-
Swelling: Inflammation around the hip area.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
X-rays: Used to assess the condition of the implant and surrounding bone.
-
MRI or CT scans: To evaluate soft tissue and detect complications like infection or bone loss.
-
Blood Tests: To check for infection markers.
-
Bone Scans: Used to identify areas of bone loss or infection.
Procedure Types or Techniques (Classification)
Revision hip replacement involves the removal of the previous hip implant and the insertion of new components. There are several techniques for revision, including:
-
Modular Components: Used to accommodate varying bone structures.
-
Cemented or Uncemented Implants: Depending on the condition of the surrounding bone, either cemented or press-fit implants may be used.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Trochanteric Bursitis: Inflammation of the bursa near the hip.
-
Sciatica: Nerve pain radiating down the leg, often mistaken for hip pain.
-
Osteoarthritis: Degenerative joint disease that affects the hip joint.
-
Infection: Infections can present as joint pain, redness, and swelling, which may be confused with other conditions.
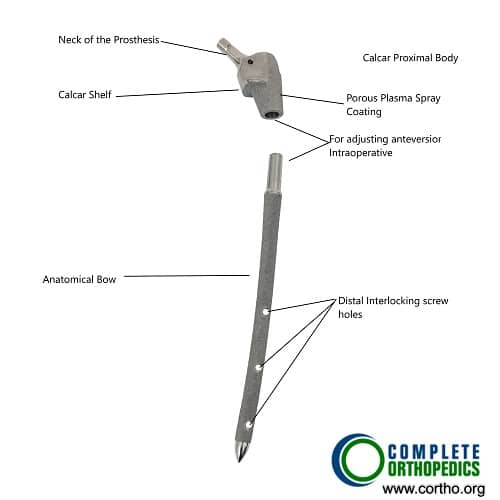
Modular femoral stem
A modular prosthetic stem allows the surgeon to compensate for excessive bone loss during extraction of the primary component. The modular stem may consist of holes for screw fixation and fully porous coating for bone ingrowth. The upper part of the prosthesis is designed to transfer load to the stronger inner of the bone.
In case of infected prosthesis, the revision surgery becomes more complicated. Decision regarding the surgery is made after assessing the duration and severity of the infection. Usually a two stage surgery is performed where in the first stage the infected implant is removed.
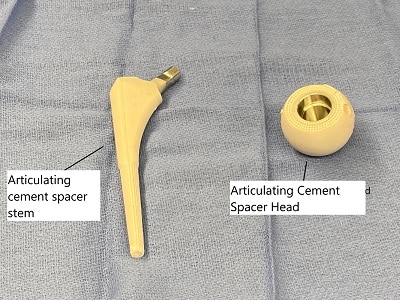
Articulating cement spacer.
The Hip joint is thoroughly washed and a cement spacer is introduced which is impregnated with antibiotics. After clearance from infection in a few weeks a second surgery is performed removing the spacer and introduction of new implants.
In a selected few cases a single stage surgery may be performed depending upon the severity of infection. Infected protestors requiring revision usually remain a long time on iv antibiotics with a very prolonged recovery period.
Treatment Options
-
Revision Surgery: The main treatment for failed hip replacements.
-
Non-surgical Management: Includes pain management, physical therapy, and anti-inflammatory medications, but these are typically not effective once the implant fails.
Recovery and What to Expect After Surgery
-
Hospital Stay: Typically 2-3 days, although some patients may require longer stays depending on complications.
-
Physical Therapy: Begins shortly after surgery to restore movement, strength, and mobility.
-
Post-Op Restrictions: Limited weight-bearing for 6-8 weeks depending on the type of implant used.
-
Full Recovery: Most patients can return to light activities within 3-6 months.
Possible Risks or Side Effects (Complications)
-
Infection: One of the most serious complications that can delay recovery.
-
Blood Clots: Deep vein thrombosis (DVT) or pulmonary embolism (PE) can occur.
-
Leg Length Discrepancy: An issue that may arise during surgery or as a result of complications.
-
Implant Loosening: The new implant can become loose over time, necessitating further revision.
-
Fractures: Bone fractures around the implant, especially in weakened bone areas.
Long-Term Outlook (Prognosis)
The long-term prognosis after revision hip replacement is generally good, with most patients experiencing significant relief from pain and improved mobility. However, the success of the revision depends on several factors, including the patient’s age, health, bone quality, and the reason for the initial implant failure.
Out-of-Pocket Cost
Medicare
CPT Code 27134 – Revision of Total Hip Replacement (Both Acetabular and Femoral Components): $448.00
Medicare Part B typically covers 80% of the approved cost for this procedure once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce patient financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which typically range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your revision hip replacement is required due to a work-related injury or complication from a prior work-related surgery, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your revision hip replacement surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
David Green required a revision of total hip replacement (CPT 27134) due to loosening of the implants. His estimated Medicare out-of-pocket cost was $448.00. Since David had supplemental insurance through AARP Medigap, his remaining balance was fully covered, leaving him with no out-of-pocket expenses for the procedure.
Frequently Asked Questions (FAQ)
Q. How long does a revision hip replacement last?
A. Revision hip replacements can last 15-20 years, but this may vary depending on factors like the patient’s activity level and health.
Q. Will I be able to walk after revision surgery?
A. Most patients can walk with assistance soon after surgery, but full recovery can take several months.
Q. Is a revision hip replacement more complicated than a primary hip replacement?
A. Yes, revision surgeries are more complex and require special planning and implants.
Summary and Takeaway
Revision hip replacement is a complex surgery that can provide excellent pain relief and restore mobility for patients with failed hip replacements. It requires careful planning and specialized techniques to ensure the best possible outcome.
Clinical Insight & Recent Findings
Despite the complexity, revision hip replacements have excellent long-term outcomes when properly planned and executed. Advances in implant design and surgical technique have significantly improved durability and patient satisfaction.
A recent study analyzing 236 revision hip replacements found that the most frequent reason for reoperation was aseptic loosening, often linked to higher body mass index, osteoporosis, and advanced age. Cement-free fixation showed better durability than cemented implants, and two-stage procedures were most effective for treating infections.
The study also emphasized the importance of a national registry to standardize reporting and improve patient outcomes. (“Study on revision hip replacements and national registry development – see PubMed.”)
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in joint replacements perform revision hip replacements. Anesthesiologists, surgical nurses, and physical therapists also play key roles in the patient’s care.
When to See a Specialist?
If you are experiencing pain, instability, or mobility issues with an existing hip implant, it may be time to consult a specialist to determine if revision surgery is necessary.
When to Go to the Emergency Room?
Seek emergency care if you experience severe pain, a dislocated hip, or signs of infection (fever, redness, swelling) after hip replacement surgery.
What Recovery Really Looks Like?
Recovery involves managing pain, restoring mobility, and following a tailored physical therapy plan. Most patients regain a good level of function within 3-6 months.
What Happens If You Delay Surgery?
Delaying revision surgery can lead to further joint deterioration, increased pain, and more complex surgery later on.
How to Prevent Recurrence or Failure?
Follow post-op instructions carefully, maintain a healthy weight, and avoid high-impact activities to prolong the life of your implant.
Nutrition and Bone or Joint Health
Adequate intake of calcium and vitamin D is essential for bone health. Avoid smoking and limit alcohol consumption to promote healing and bone health.
Activity and Lifestyle Modifications
Engage in low-impact activities and follow your surgeon’s recommendations to maintain joint function and prevent implant failure.
Do you have more questions?
What is revision hip replacement surgery?
Revision hip replacement surgery is a procedure performed to replace a previously implanted artificial hip joint that has either worn out, become damaged, or failed for various reasons.
When might someone need revision hip replacement surgery?
Revision hip replacement surgery may be necessary due to factors such as loosening of the implant, infection, fracture around the implant, instability, or wear and tear of the artificial joint over time.
What are the signs that a hip replacement may need revision?
Signs indicating a potential need for revision hip replacement include persistent pain, instability or dislocation of the hip, difficulty walking or bearing weight, and evidence of implant failure on imaging studies.
How is revision hip replacement surgery different from primary hip replacement?
Revision hip replacement surgery is more complex than primary hip replacement as it involves removing the existing implant, addressing any bone loss or structural issues, and then replacing it with a new implant.
What are the risks associated with revision hip replacement surgery?
Risks of revision hip replacement surgery include infection, blood clots, nerve injury, fracture, dislocation, and the need for further revision surgeries in the future.
How long does it take to recover from revision hip replacement surgery?
Recovery time from revision hip replacement surgery varies depending on factors such as the patient’s overall health, the extent of the surgery, and any complications encountered during the procedure. Generally, it may take several months to fully recover.
What is the success rate of revision hip replacement surgery?
The success rate of revision hip replacement surgery depends on various factors such as the reason for revision, the surgeon’s skill, and the patient’s overall health. Generally, success rates are high, with many patients experiencing significant improvement in symptoms and function.
Can all hip replacement implants be revised?
While most hip replacement implants can be revised, some factors such as implant design, fixation method, and bone quality may affect the feasibility and success of revision surgery.
How do I know if I’m a candidate for revision hip replacement surgery?
Candidates for revision hip replacement surgery typically undergo a thorough evaluation by an orthopedic surgeon, including physical examination, imaging studies, and medical history review, to determine the most appropriate course of treatment.
Are there alternatives to revision hip replacement surgery?
Depending on the specific circumstances, alternatives to revision hip replacement surgery may include conservative management with medications, physical therapy, or other non-surgical interventions. However, in many cases, revision surgery may be the most effective option for addressing implant failure or complications.
Will revision hip replacement surgery relieve all of my hip pain?
While revision hip replacement surgery aims to alleviate hip pain and improve function, it may not completely eliminate all symptoms, particularly if there are underlying issues such as nerve damage or extensive bone loss.
What type of anesthesia is used for revision hip replacement surgery?
Revision hip replacement surgery is typically performed under general anesthesia, although regional anesthesia techniques such as spinal or epidural anesthesia may also be used in some cases.
How long does revision hip replacement surgery take?
The duration of revision hip replacement surgery varies depending on factors such as the complexity of the case and any unforeseen complications, but it generally takes several hours to complete.
Will I need physical therapy after revision hip replacement surgery?
Yes, physical therapy is an essential component of rehabilitation following revision hip replacement surgery. A structured exercise program helps improve strength, range of motion, and functional mobility.
What can I expect during the recovery period after revision hip replacement surgery?
During the recovery period, patients can expect to gradually regain mobility and function with the help of physical therapy. Pain and discomfort are common initially but should improve over time
Are there any restrictions on activities after revision hip replacement surgery?
While activity restrictions may vary depending on individual circumstances and the surgeon’s recommendations, patients are generally advised to avoid high-impact activities and heavy lifting to prevent implant failure or complications.
Will I need to take medication after revision hip replacement surgery?
Depending on the individual patient’s needs, medications such as pain relievers, antibiotics, and blood thinners may be prescribed following revision hip replacement surgery to manage pain, prevent infection, and reduce the risk of blood clots.
How often will I need to follow up with my surgeon after revision hip replacement surgery?
Follow-up appointments with the surgeon are typically scheduled at regular intervals following revision hip replacement surgery to monitor healing, assess progress, and address any concerns or complications that may arise.
Can revision hip replacement surgery be performed using minimally invasive techniques?
Minimally invasive techniques may be utilized in some cases of revision hip replacement surgery, depending on factors such as the patient’s anatomy and the complexity of the revision. However, not all cases are suitable for minimally invasive approaches.
What factors affect the success of revision hip replacement surgery?
Factors influencing the success of revision hip replacement surgery include the surgeon’s experience and skill, the reason for revision, the condition of the bone and surrounding tissues, and the patient’s overall health and compliance with postoperative instructions.
Will I need blood transfusions during or after revision hip replacement surgery?
Blood transfusions may be necessary during or after revision hip replacement surgery, particularly in cases where there is significant blood loss. Your surgeon will discuss the potential need for transfusions and address any concerns you may have.
How can I minimize the risk of complications during and after revision hip replacement surgery?
Following your surgeon’s preoperative instructions, maintaining good overall health, and adhering to postoperative guidelines such as activity restrictions, medication regimens, and physical therapy can help minimize the risk of complications and promote a successful outcome.
What should I do if I experience unexpected symptoms or complications after revision hip replacement surgery?
If you experience unexpected symptoms or complications after revision hip replacement surgery, such as increased pain, swelling, fever, or difficulty with mobility, it is important to contact your surgeon promptly for evaluation and management. Early detection and intervention can help prevent further complications and promote optimal recovery.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
