Total Knee Replacement
Total hip replacement (THR), also known as total hip arthroplasty, is one of the most successful surgeries in modern medicine. It is designed to relieve pain, improve mobility, and restore function for patients suffering from hip joint conditions, such as arthritis, fractures, or other degenerative diseases. Over the years, advancements in surgical techniques and implant technology have dramatically improved the effectiveness of THR, allowing patients to return to their normal activities and enjoy a pain-free life.
How Common It Is and Who Gets It? (Epidemiology)
Every year, more than 450,000 total hip replacements are performed in the United States. The majority of patients undergoing this surgery are between the ages of 50 and 80, with osteoarthritis being the most common reason for the procedure. Patients with chronic hip pain, restricted mobility, and severe arthritis may require this surgery when other conservative treatments, such as medications or physical therapy, fail to provide relief.
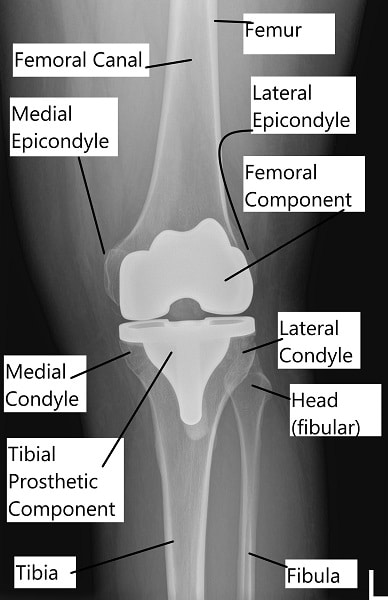
Total knee replacement X-ray
Why It Happens – Causes (Etiology and Pathophysiology)
The most common cause of hip pain and degeneration is osteoarthritis. In this condition, the cartilage in the hip joint breaks down, causing the bones to rub together and resulting in pain and stiffness. Other causes of hip joint degeneration include:
-
Rheumatoid arthritis: An autoimmune disease that causes inflammation and damage to the hip joint.
-
Post-traumatic arthritis: Arthritis following a previous hip injury or fracture.
-
Avascular necrosis: The loss of blood supply to the femoral head, leading to bone death.
-
Hip fractures: Severe fractures of the femoral head or acetabulum may lead to joint dysfunction and arthritis.
How the Body Part Normally Works? (Relevant Anatomy)
The hip joint is a ball-and-socket joint formed by:
-
The femoral head (the ball) at the upper end of the femur (thigh bone).
-
The acetabulum (the socket), part of the pelvic bone.
The surfaces of the ball and socket are lined with smooth articular cartilage that cushions the bones and allows for smooth movement. The joint is stabilized by ligaments and muscles surrounding the hip, providing both mobility and support.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with hip arthritis typically experience:
-
Severe pain during weight-bearing activities like walking, standing, or climbing stairs.
-
Stiffness in the hip, leading to difficulty bending or lifting the leg.
-
Pain at rest, especially at night or after prolonged sitting.
-
Swelling and discomfort around the hip joint.
-
Difficulty performing daily tasks like putting on shoes, sitting in a chair, or getting in and out of a car.
How Doctors Find the Problem? (Diagnosis and Imaging)
A comprehensive diagnosis includes:
-
Physical examination: The surgeon will assess the hip’s range of motion, strength, and alignment.
-
X-rays: These are crucial for visualizing the degree of joint degeneration and bone changes associated with arthritis.
-
MRI or CT scans: These can provide detailed images of both bone and soft tissues, especially in cases of complex hip conditions.
-
Bone scans: Sometimes used to assess the extent of damage to the bone.
Procedure Types or Techniques (Classification)
There are different approaches for total hip replacement surgery:
-
Cemented vs. Cementless: The femoral stem and acetabular components can either be press-fit into the bone or secured with bone cement.
-
Minimally invasive techniques: Smaller incisions and specialized tools are used to minimize trauma to surrounding tissues.
-
Anterior vs. Posterior Approaches: The surgery can be performed through various access points, depending on the surgeon’s preference and patient anatomy.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Trochanteric bursitis: Inflammation of the bursa on the outer side of the hip.
-
Sciatica: Nerve pain radiating from the lower back to the hip and leg.
-
Osteonecrosis: Bone death due to interrupted blood supply to the femoral head.
-
Hip labral tear: Damage to the cartilage around the hip socket, causing pain and instability.
Treatment Options
Conservative treatments: Medications, physical therapy, weight management, and joint injections are often used before considering surgery.
Surgical treatment: Total hip replacement surgery is recommended when conservative treatments fail.
Recovery and What to Expect After Surgery
-
Hospital Stay: Most patients stay in the hospital for 1-3 days, depending on their health and recovery progress.
-
Physical Therapy: Therapy typically begins the day after surgery to help with mobility, strength, and reducing the risk of complications like blood clots.
-
Pain Management: A multimodal approach (including non-opioid medications) helps manage pain during recovery.
-
Full recovery: Most patients regain normal function and mobility within 3-6 months, although full recovery may take longer in older patients or those with other health conditions.
Possible Risks or Side Effects (Complications)
-
Infection: Infection can occur in the wound or around the prosthesis, potentially requiring more surgery.
-
Blood clots: DVT or pulmonary embolism can occur, which is why patients are encouraged to move as soon as possible.
-
Dislocation: The prosthesis may dislocate, particularly in the first few months after surgery.
-
Leg length discrepancy: Some patients experience minor length differences between legs after surgery.
-
Implant loosening: Over time, the implant may loosen due to wear, necessitating a revision surgery.
Long-Term Outlook (Prognosis)
With proper care, most patients experience significant pain relief and an improved ability to perform daily activities. The implants typically last 15-20 years, although some patients, particularly younger, more active individuals, may require a revision surgery if the implant wears out or loosens.
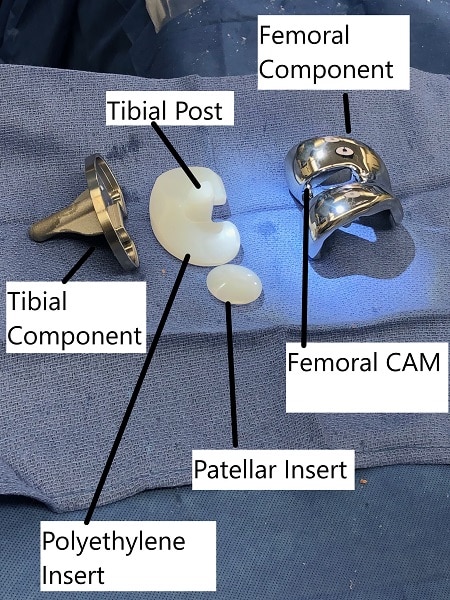
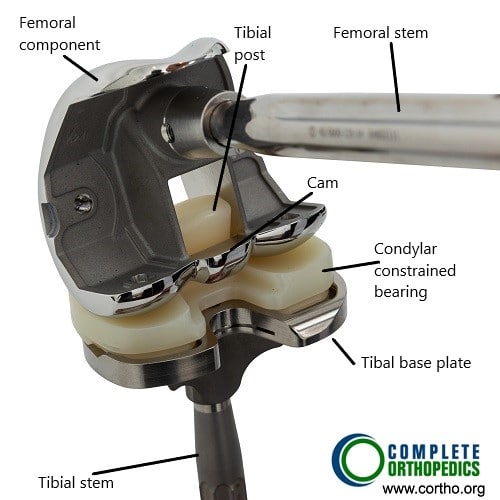
Prosthetic parts of total knee replacement
Out-of-Pocket Costs
Medicare
CPT Code 27130 – Primary Total Hip Arthroplasty (Replacement of Both Acetabulum and Femoral Head): $303.45
CPT Code 27132 – Conversion to Total Hip Arthroplasty (Conversion of Prior Hip Surgery to Total Hip): $394.09
CPT Code 27134 – Revision THA (Both Components, Acetabular and Femoral): $448.00
CPT Code 27137 – Revision THA (Acetabular Component Only): $345.69
CPT Code 27138 – Revision THA (Femoral Component Only): $359.01
CPT Code 27125 – Hemiarthroplasty (Partial Hip Replacement, Replacement of Femoral Head Only): $268.14
Medicare Part B typically covers 80% of the approved cost for these procedures once your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce patient costs.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it serves as a secondary payer. These plans generally cover any remaining balance, including coinsurance or small deductibles, which typically range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your hip replacement or revision surgery is required due to a work-related injury, Workers’ Compensation will cover all associated medical expenses, including surgery, rehabilitation, and follow-up care. You will not have any out-of-pocket expenses, as the employer’s insurance carrier directly covers all approved treatments.
No-Fault Insurance
If your hip surgery is needed due to an automobile accident, No-Fault Insurance will typically cover the full cost of treatment, including surgery and postoperative care. The only potential out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Thomas Johnson required a primary total hip arthroplasty (CPT 27130) due to arthritis, with an estimated Medicare out-of-pocket cost of $303.45. Later, he required a revision of both components (CPT 27134) with an estimated out-of-pocket cost of $448.00. Since Thomas had supplemental insurance through Blue Cross Blue Shield, both amounts were fully covered, leaving him with no out-of-pocket expenses for the procedures.
Frequently Asked Questions (FAQ)
Q. How long will my new hip last?
A. Most implants last 15-20 years, with some patients experiencing even longer durability.
Q. Can I run after hip replacement?
A. High-impact activities such as running are discouraged after surgery. Low-impact activities like walking, swimming, and cycling are ideal.
A recent study examined the impact of osteoporosis on outcomes following total hip arthroplasty (THA), focusing on bone mineral density (BMD) and the associated risks of complications such as periprosthetic fractures (PPFs) and implant loosening. The research highlights that osteoporosis and osteopenia are prevalent among THA candidates, particularly the elderly, with a significant percentage of osteoporosis cases remaining undiagnosed preoperatively. The study found that osteoporotic patients are at an increased risk for poor surgical outcomes, including higher rates of PPFs and revision surgeries. Additionally, the study emphasizes the importance of preoperative screening and appropriate treatment to mitigate these risks, noting that the use of cemented femoral stems can reduce the incidence of PPFs in osteoporotic patients. The findings underline the need for comprehensive management strategies, including pharmacological interventions and optimal surgical techniques, to improve outcomes in this high-risk population. Study of osteoporosis in THA – See PubMed.
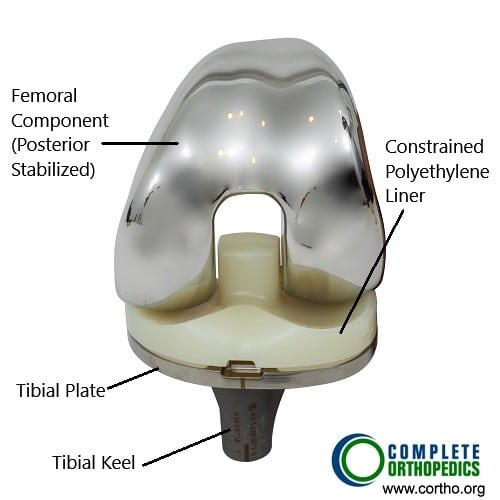
Total knee replacement components (front view)
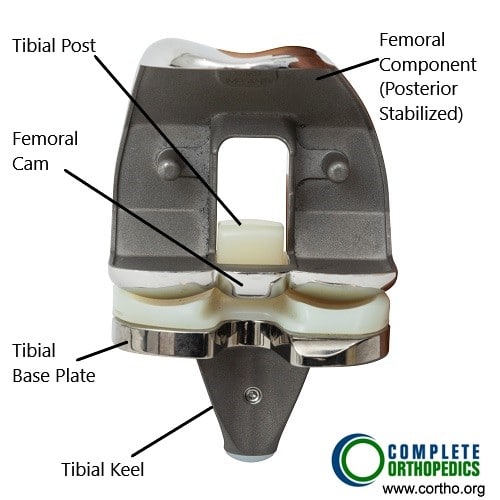
Total knee replacement components (back view)
The above images show the prosthetic knee replacement components from the front and the back. The femoral component (posterior stabilized) has a cam mechanism which allows posterior translation of the femur on the tibial post of the bearing surface. The femoral rollback aids in achieving deeper flexion which in a normal knee is done by the knee ligaments. The polyethylene insert is made of highly cross linked polyethylene, which is resistant to wear and tear. The keel of the tibial component is fixed in the upper part of the shin bone using bone cement.
Revision knee modular components
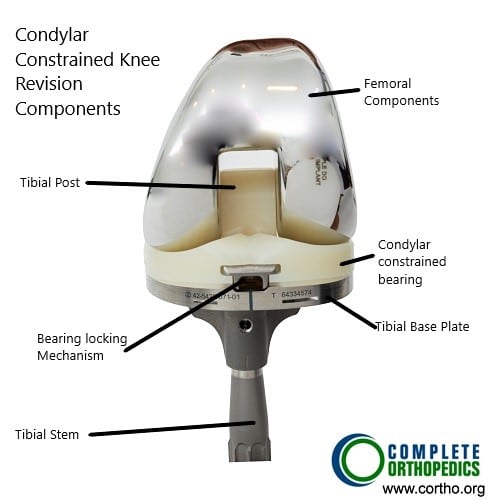
Revision knee modular components
The modular components shown in the images above are used in revision knee surgery or complex knee replacement. Depending upon the knee anatomy and bone loss, the surgeon is able to achieve greater stability of the prosthetic implant using modular components.
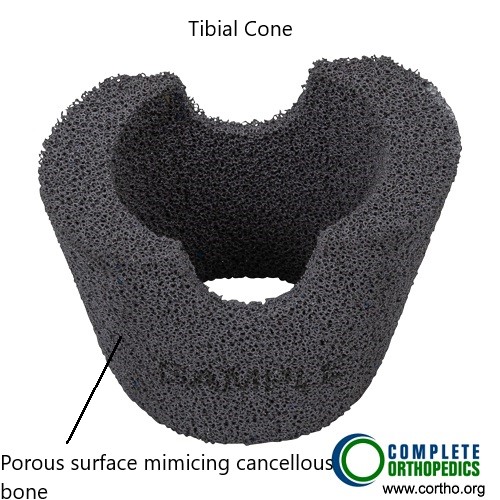
Tibial cone augment
Metal cone resembling trabecular bone may be used to fill in bone gaps encountered in the metaphyseal region intraoperatively. The trabecular surface pattern of the tibial cone ensures biological union of the component.
Summary and Takeaway
Total hip replacement is a highly effective procedure for individuals suffering from severe hip pain due to arthritis or other joint diseases. The surgery can dramatically improve quality of life by reducing pain, increasing mobility, and enabling patients to return to their normal activities.
Clinical Insight & Recent Findings
Who Performs This Surgery? (Specialists and Team Involved)
Orthopedic surgeons specializing in joint replacements typically perform total hip replacement surgeries, supported by a team of anesthesiologists, nurses, and physical therapists.
When to See a Specialist?
If hip pain is interfering with your daily life and conservative treatments have failed to provide relief, it may be time to consult an orthopedic surgeon for a thorough evaluation.
When to Go to the Emergency Room?
Seek emergency care if you experience severe pain, swelling, or signs of infection, such as redness or fever, after surgery.
What Recovery Really Looks Like?
Most patients can begin walking with assistance the day after surgery. Full recovery can take up to 6 months, with significant improvements in the first few months.
What Happens If You Delay Surgery?
Delaying surgery may lead to further joint damage, increased pain, and complications that could make the procedure more difficult.
How to Prevent Recurrence or Failure?
Maintain a healthy weight, avoid high-impact activities, and follow your surgeon’s recommendations to ensure the longevity of the implant.
Nutrition and Bone or Joint Health
Adequate intake of calcium and vitamin D is essential for bone health during the recovery period.
Activity and Lifestyle Modifications
Engage in low-impact activities and avoid excessive weight-bearing or high-impact sports to preserve the health of your new hip.
Do you have more questions?
How soon after knee replacement surgery can complications typically arise?
Complications after knee replacement surgery can arise at various times during the postoperative period, ranging from the immediate postoperative period to months or even years after surgery. It’s essential to remain vigilant for signs and symptoms of complications and seek prompt medical attention if any concerns arise.
Are there any specific precautions or considerations for patients with certain medical conditions (e.g., diabetes, heart disease) undergoing knee replacement surgery?
Patients with medical conditions may require additional preoperative evaluation and optimization to reduce the risk of complications during and after knee replacement surgery. Close coordination between the orthopedic surgeon and other medical specialists is essential to ensure safe and successful outcomes.
What factors should patients consider when selecting a surgeon and hospital for knee replacement surgery?
Patients should consider factors such as surgeon experience, hospital reputation, surgical volume, complication rates, patient satisfaction scores, and access to comprehensive pre- and post-operative care when choosing where to undergo knee replacement surgery.
How does prehabilitation (pre-operative rehabilitation) contribute to better outcomes following knee replacement surgery, and what exercises are typically included in prehabilitation programs?
Prehabilitation aims to optimize patients’ physical and mental health before surgery, leading to improved post-operative recovery and functional outcomes. Exercises often include strengthening, flexibility, and cardiovascular conditioning tailored to individual needs.
What are the potential risks and benefits of simultaneous bilateral knee replacement surgery compared to staged procedures?
Simultaneous bilateral knee replacement offers the advantage of a single anesthesia exposure and shorter overall recovery time but may carry increased risks such as higher blood loss and complications related to immobility.
Are there any emerging technologies or advancements in knee replacement surgery that patients should be aware of?
Emerging technologies such as patient-specific implants, 3D printing, and advanced surgical navigation systems are being explored to further improve the precision and outcomes of knee replacement surgery.
What are the potential risks and complications associated with knee replacement surgery?
Knee replacement surgery, like any surgical procedure, carries risks such as infection, blood clots, nerve damage, implant failure, stiffness, and persistent pain.
How long does it typically take to recover from knee replacement surgery, and what is the rehabilitation process like?
Recovery time can vary, but most patients undergo several weeks of physical therapy to regain strength, mobility, and function in the replaced knee.
Are there any restrictions or limitations on activities following knee replacement surgery?
While patients can typically resume low-impact activities like walking and swimming, high-impact activities such as running and jumping may be discouraged to prevent implant wear and tear.
What factors determine the success rate of knee replacement surgery, and how can patients optimize their outcomes?
Success rates depend on factors such as patient age, overall health, severity of knee damage, surgical technique, implant selection, and adherence to post-operative rehabilitation protocols.
Are there alternatives to traditional knee replacement surgery, such as partial knee replacement or minimally invasive procedures?
Yes, alternatives include partial knee replacement for localized knee arthritis and minimally invasive techniques that aim to preserve more healthy tissue and facilitate quicker recovery.
What is the role of robotic-assisted surgery in knee replacement procedures, and how does it differ from traditional approaches?
Robotic-assisted surgery utilizes advanced technology to enhance precision and accuracy in implant placement, potentially improving outcomes and reducing complications compared to traditional techniques.
Can knee replacement surgery be performed on both knees simultaneously, or is it typically done one at a time?
While simultaneous bilateral knee replacement can be considered for select patients, most individuals undergo staged procedures, addressing one knee at a time to minimize post-operative complications and facilitate rehabilitation.
How long do knee implants typically last, and what factors can affect their longevity?
Knee implants can last 15-20 years or longer, but their durability may be influenced by factors such as patient activity level, implant design, material quality, and surgical technique.
Can knee replacement surgery be performed in younger patients, and are there any special considerations for this population?
Knee replacement in younger patients may present challenges due to the need for long-term implant durability and potential revision surgeries over their lifetime. Careful patient selection and counseling are essential.
What are the potential complications of delaying knee replacement surgery, and when is the optimal time to consider surgery?
Delaying surgery may lead to worsening pain, functional limitations, joint deformity, and compromised outcomes. The optimal timing for surgery depends on the individual’s symptoms, functional status, and response to conservative treatments.
Are there any lifestyle modifications or preventive measures that can help delay or minimize the need for knee replacement surgery?
Lifestyle modifications such as weight management, regular exercise, joint protection techniques, and appropriate footwear may help alleviate knee pain and delay the progression of arthritis, reducing the need for surgery.
What are the differences between total knee replacement and partial knee replacement, and how is the appropriate procedure determined?
Total knee replacement involves replacing the entire knee joint, while partial knee replacement addresses only the damaged compartment. The choice between procedures depends on the extent and location of arthritis and the patient’s anatomy.
What types of anesthesia are used for knee replacement surgery, and what are the associated risks and benefits?
Knee replacement surgery can be performed under general anesthesia, regional anesthesia (such as spinal or epidural), or a combination of both. The choice depends on patient factors and surgical preferences, with each option carrying its own risks and benefits.
Are there any factors that may increase the risk of complications or adverse outcomes following knee replacement surgery?
Factors such as advanced age, obesity, smoking, diabetes, heart disease, and certain medications may increase the risk of complications and warrant careful preoperative evaluation and optimization.
What are the most common reasons for knee replacement revision surgery, and how are complications addressed?
Reasons for revision surgery include infection, implant loosening, instability, wear and tear, and persistent pain. Revision procedures aim to address complications and restore function, often requiring more complex surgical techniques.
How does the choice of implant type (e.g., fixed-bearing vs. mobile-bearing) affect outcomes and longevity in knee replacement surgery?
Implant selection depends on factors such as patient age, activity level, and surgeon preference. Both fixed-bearing and mobile-bearing designs have shown favorable outcomes, with differences in wear patterns and range of motion.
Are there any complementary or alternative therapies that can help manage knee pain and improve function without surgery?
Complementary therapies such as acupuncture, massage, physical therapy, and dietary supplements may provide symptomatic relief and improve joint function, although their efficacy varies among individuals.
How does knee osteoarthritis differ from other types of arthritis, and what are the treatment options specific to this condition?
Knee osteoarthritis is characterized by the breakdown of cartilage in the knee joint, leading to pain, stiffness, and loss of function. Treatment options include lifestyle modifications, medications, injections, physical therapy, and surgical interventions like knee replacement.
Can knee injuries such as ACL tears or meniscus tears be effectively treated without surgery, and what factors influence the decision for surgical intervention?
While some knee injuries may heal with conservative measures like rest, physical therapy, and bracing, surgical intervention may be necessary for severe or unstable injuries that compromise joint stability and function. Individualized treatment plans are based on factors such as the severity of injury, patient activity level, and treatment goals.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
