Cervical Spine Stenosis
Cervical spine stenosis is a condition in which the spaces within the neck portion of the spine become narrowed, putting pressure on the spinal cord or nerve roots. This narrowing often results from natural aging and gradual wear and tear of the spinal structures. While some people experience only mild symptoms, others may develop significant pain, numbness, or weakness that affects daily activities.
How Common It Is and Who Gets It? (Epidemiology)
Cervical spinal stenosis is most common in adults over the age of 50. The condition develops gradually over time as discs lose height, ligaments thicken, and joints enlarge. People born with a naturally narrow spinal canal (congenital stenosis) are at higher risk. Other factors—such as previous injuries, arthritis, or prior spine surgery—can also contribute.
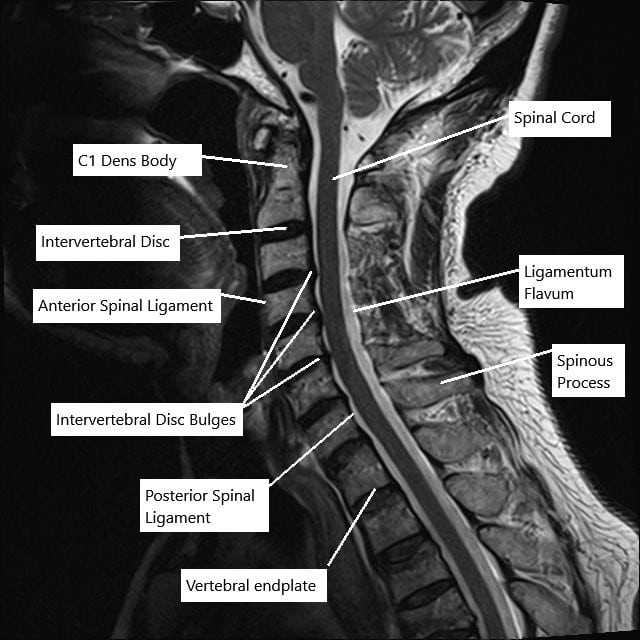
MRI of the cervical spine in sagittal section showing disc herniations.
Why It Happens – Causes (Etiology and Pathophysiology)
The cervical spine can narrow for many reasons, most related to aging:
-
Arthritis: Wear and tear of joints leads to bone spurs that reduce space for the spinal cord.
-
Disc degeneration or herniation: Flattened or bulging discs can press against nerves.
-
Thickened ligaments: The bands that support the spine may stiffen and buckle into the spinal canal.
-
Malalignment: A slipped vertebra (spondylolisthesis) can further narrow space.
-
Trauma: Fractures or dislocations from accidents can cause direct compression.
-
Genetic or metabolic diseases: Conditions such as Paget’s disease, achondroplasia, or fluorosis may also lead to narrowing.
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine consists of seven vertebrae that protect the spinal cord and allow head and neck motion. Between the vertebrae are discs that absorb shock and provide flexibility. Small openings between bones (foramina) let nerves branch from the spinal cord to the shoulders, arms, and hands.
When the canal or foramina become smaller, the spinal cord or nerves can be squeezed, leading to pain and neurological symptoms.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms depend on how much the nerves or spinal cord are compressed. Common signs include:
-
Neck pain or stiffness
-
Radiating pain into the shoulders or arms
-
Tingling, numbness, or weakness in the arms or hands
-
Loss of coordination, clumsiness, or difficulty with fine motor skills
-
Unsteady walking or frequent tripping
-
In severe cases, loss of bladder or bowel control
Mild cases may cause only occasional discomfort, while advanced stenosis can lead to significant weakness and functional loss.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed medical history and neurological examination. The doctor will test strength, reflexes, balance, and sensation.
Imaging studies may include:
-
X-rays: Show bone alignment and narrowing between vertebrae.
-
CT scans: Provide detailed views of bone spurs and ligament thickening.
-
MRI scans: Offer the best look at soft tissues, discs, and the spinal cord itself.
MRI findings help determine whether symptoms come from nerve or spinal cord compression and guide treatment decisions.
Classification
Cervical spine stenosis can be categorized by its location:
-
Central stenosis: Narrowing of the spinal canal that compresses the spinal cord.
-
Lateral recess stenosis: Narrowing near where the nerve roots exit.
-
Foraminal stenosis: Compression within the small openings where nerves leave the spine.
Severity may be graded as mild, moderate, or severe, based on how much space remains for the neural structures.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic cervical stenosis include:
-
Herniated discs without significant narrowing
-
Peripheral neuropathy
-
Multiple sclerosis or other nerve disorders
-
Shoulder or arm joint disease
-
Spinal infections or tumors
Proper imaging and neurological evaluation help distinguish these conditions.
Treatment Options
Non-Surgical Care
Most patients begin with conservative treatment, which may include:
-
Medications: Anti-inflammatory drugs or muscle relaxants to ease pain and stiffness.
-
Physical therapy: Exercises to strengthen neck and shoulder muscles and improve posture.
-
Heat or cold therapy: To relieve muscle tension.
-
Injections: Corticosteroid injections may temporarily reduce inflammation and pain.
-
Lifestyle adjustments: Avoiding heavy lifting and maintaining good posture during daily activities.
Surgical Care
Surgery is considered when conservative treatment fails or when there is significant spinal cord compression. The goal is to relieve pressure and stabilize the spine.
Common procedures include:
-
Laminotomy: Removal of a small portion of bone to increase space.
-
Laminectomy: Removal of the entire lamina (back part of the vertebra) to decompress the spinal cord.
-
Foraminotomy: Widening of the openings where nerves exit the spine.
-
Laminoplasty: Creating a hinge to enlarge the canal while keeping bone intact.
-
Anterior cervical discectomy and fusion (ACDF): Removing damaged discs and stabilizing the spine from the front.
The approach depends on the number of affected levels and whether alignment or stability issues are present.

Rasp used in ACDF

ACDF Plate with screws
The images above show a rasp used during the anterior decompression and fusion surgery. The rasp is used to prepare the end plate for insertion of bone cage and subsequent fixation of the vertebrae using the plate shown above.
Recovery and What to Expect After Treatment
-
Non-surgical cases: Most patients experience gradual improvement within weeks with physical therapy and medication.
-
After surgery: Patients usually stay in the hospital for 1–3 days. Light activity can begin soon after, with full recovery taking several months.
Physical therapy focuses on gentle stretching, strengthening, and posture correction. Long-term results are excellent when the spinal cord and nerves are decompressed early.
Possible Risks or Side Effects (Complications)
As with any spine procedure, complications are rare but may include:
-
Infection or bleeding
-
Nerve or spinal cord injury
-
Fusion failure or hardware problems
-
Difficulty swallowing or hoarseness (temporary after anterior surgery)
-
Persistent pain or stiffness
Proper technique, medical optimization, and adherence to recovery plans help minimize these risks.
Long-Term Outlook (Prognosis)
Most patients achieve significant improvement in pain, strength, and coordination after appropriate treatment. Surgery is highly effective in stopping progression and preventing further nerve damage. However, long-standing compression may cause lasting weakness or numbness even after decompression.
Out-of-Pocket Costs
Medicare
CPT Code 22551 – Anterior Cervical Discectomy and Fusion (ACDF): $417.50
CPT Code 63081 – Corpectomy (Anterior Decompression): $433.45
CPT Code 63045 – Posterior Laminectomy (Decompression): $319.26
CPT Code 22600 – Posterior Cervical Fusion: $322.92
CPT Code 63050 – Laminoplasty: $362.34
For Medicare beneficiaries, the program generally pays 80% of the approved amount after the annual deductible is met. The patient is responsible for the remaining 20%. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield typically cover this 20%, ensuring minimal or no out-of-pocket costs for Medicare-approved cervical spine surgeries. These supplemental plans coordinate directly with Medicare to close the cost gap, allowing patients to focus on recovery without financial stress.
If you have a secondary insurance plan—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare has processed the claim. After your deductible is satisfied, the secondary plan may cover the remaining co-insurance or balance. Some secondary plans have their own small deductible, typically between $100 and $300, depending on the specific policy and whether the surgery is performed in-network.
Workers’ Compensation
If your cervical spine stenosis was caused or worsened by a work-related injury, Workers’ Compensation will pay all medical and surgical costs related to the treatment. This includes decompression, corpectomy, fusion, or laminoplasty procedures. Patients will have no out-of-pocket expenses for covered services under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your cervical stenosis resulted from a motor vehicle accident, No-Fault Insurance will cover all necessary diagnostic, surgical, and hospital costs associated with the procedure. The only potential out-of-pocket expense is a small deductible, depending on your individual policy.
Example
Karen, a 62-year-old patient with severe cervical spine stenosis, underwent a corpectomy (CPT 63081) and posterior fusion (CPT 22600) to relieve spinal cord compression. Her estimated Medicare out-of-pocket costs were $433.45 and $322.92, respectively. Because Karen had supplemental insurance through Medigap, the remaining 20% coinsurance was fully covered, leaving her with no out-of-pocket expenses for her surgery.
Frequently Asked Questions (FAQ)
Q. Is cervical stenosis always progressive?
A. Not always. Some patients remain stable for years with mild symptoms.
Q. Can it heal on its own?
A. While narrowing cannot reverse, symptoms often improve with therapy and lifestyle changes.
Q. Is surgery safe?
A. Yes. When performed by experienced spine surgeons, success rates are high, and complications are uncommon.
Q. How long will I need physical therapy?
A. Most patients benefit from 4–8 weeks of guided exercises after treatment or surgery.
Summary and Takeaway
Cervical spine stenosis occurs when the spinal canal narrows and presses on nerves or the spinal cord. While most cases respond to medication, therapy, and posture correction, surgery may be needed to relieve severe compression. Early diagnosis and personalized treatment allow most people to return to normal activities with minimal limitations.
Clinical Insight & Recent Findings
A recent study examined the outcomes of combined carpal and cubital tunnel decompression in patients who also had mild to moderate cervical spine stenosis. Among 100 participants, those who underwent simultaneous decompression of both tunnels reported significantly lower pain severity and interference scores, as well as better functional outcomes, compared with patients treated for a single site of nerve compression.
The combined procedure resulted in a median pain score of 1/10 and a QuickDASH disability score of only 5%, indicating improved hand function and reduced discomfort. The findings suggest that treating multiple compression sites concurrently can enhance recovery and quality of life for patients with both peripheral nerve entrapments and cervical stenosis, challenging the traditional “double crush” concept that predicts poorer outcomes when spinal pathology coexists.
However, researchers noted that larger studies are needed to confirm these results and optimize surgical strategies. (Study of combined decompression in cervical spine stenosis – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Cervical spine stenosis is treated by orthopedic spine surgeons or neurosurgeons, supported by physical therapists, pain specialists, and rehabilitation teams.
When to See a Specialist?
Consult a specialist if you have:
-
Persistent or worsening neck pain
-
Tingling, weakness, or numbness in your arms or hands
-
Trouble with balance or fine motor tasks
When to Go to the Emergency Room?
Seek immediate care if you experience:
-
Sudden paralysis or severe weakness
-
Loss of bladder or bowel control
-
Severe neck pain following injury or trauma
What Recovery Really Looks Like?
Most patients regain mobility and pain relief within months of treatment. Some may experience mild stiffness or sensitivity, which improves with ongoing therapy and proper ergonomics.
What Happens If You Ignore It?
Untreated cervical stenosis can lead to irreversible spinal cord injury, chronic pain, or paralysis. Prompt diagnosis prevents permanent damage.
How to Prevent It?
-
Maintain good posture
-
Avoid smoking and repetitive strain
-
Strengthen neck and shoulder muscles
-
Address neck injuries early
-
Keep a healthy body weight and stay active
Nutrition and Bone or Joint Health
Eating foods rich in calcium, vitamin D, and protein supports bone and disc health. Adequate hydration helps keep spinal discs flexible.
Activity and Lifestyle Modifications
Gentle exercises such as swimming, yoga, or walking maintain neck flexibility. Avoid high-impact activities or heavy lifting, and use ergonomic chairs and pillows for support.
Do you have more questions?
Can cervical spinal stenosis be completely cured?
While cervical spinal stenosis cannot be completely cured, symptoms can be managed effectively with a combination of non-surgical and surgical treatments depending on the severity of the condition.
Are there any activities that should be avoided with cervical spinal stenosis?
Activities that put excessive strain on the neck, such as heavy lifting, high-impact sports, and certain exercises, should be avoided to prevent exacerbation of symptoms.
How long does it take to recover from surgery for cervical spinal stenosis?
Recovery time can vary, but generally, patients may need several weeks to a few months to recover from cervical spine surgery, with physical therapy playing a crucial role in the rehabilitation process.
Is physical therapy always required after surgery for cervical spinal stenosis?
Yes, physical therapy is typically recommended after surgery to help restore mobility, strengthen muscles, and ensure proper healing.
Can cervical spinal stenosis cause headaches?
Yes, cervical spinal stenosis can sometimes cause headaches, particularly if the stenosis affects the upper cervical vertebrae.
Are there any long-term effects of cervical spinal stenosis on daily life?
Long-term effects can include chronic pain, reduced mobility, and in severe cases, neurological deficits. However, with proper treatment, many people can manage their symptoms and maintain a good quality of life.
How is cervical spinal stenosis different from lumbar spinal stenosis?
Cervical spinal stenosis affects the neck region of the spine, while lumbar spinal stenosis affects the lower back. Symptoms and potential complications differ based on the location of the stenosis.
Can lifestyle changes help manage cervical spinal stenosis symptoms?
Yes, maintaining a healthy weight, regular low-impact exercise, good posture, and ergonomic adjustments at work can help manage symptoms.
What is the success rate of surgery for cervical spinal stenosis?
Surgery for cervical spinal stenosis has a high success rate, with many patients experiencing significant relief from symptoms. Success rates can range from 70% to 90%, depending on the procedure and patient condition.
Can cervical spinal stenosis lead to paralysis?
In severe cases where the spinal cord is significantly compressed, cervical spinal stenosis can lead to paralysis, but this is relatively rare with early and appropriate treatment.
Are there any non-pharmacological treatments for pain management in cervical spinal stenosis?
Yes, non-pharmacological treatments include physical therapy, acupuncture, chiropractic care, and cognitive-behavioral therapy for pain management.
What role does genetics play in cervical spinal stenosis?
Genetics can play a role, particularly if there is a family history of spinal conditions or congenital spinal canal narrowing.
Is there a way to prevent cervical spinal stenosis?
While you cannot prevent the aging process, you can reduce the risk by maintaining a healthy lifestyle, avoiding neck injuries, and managing underlying conditions like arthritis.
Can cervical spinal stenosis cause sleep problems?
Yes, pain and discomfort from cervical spinal stenosis can interfere with sleep, making it difficult to find a comfortable position.
How often should someone with cervical spinal stenosis see a doctor?
Regular follow-ups every six months to a year, or more frequently if symptoms worsen, are recommended to monitor the condition and adjust treatment as needed.
Are there any alternative therapies that can help with cervical spinal stenosis?
Alternative therapies such as acupuncture, yoga, massage, and herbal supplements may provide symptom relief for some individuals, but should be discussed with a healthcare provider.
Can cervical spinal stenosis cause dizziness or vertigo?
Yes, cervical spinal stenosis can sometimes cause dizziness or vertigo, particularly if the blood flow to the brain is affected.
What imaging tests are best for diagnosing cervical spinal stenosis?
MRI is the most effective imaging test for diagnosing cervical spinal stenosis as it provides detailed images of the spinal cord and nerves. CT scans and X-rays are also useful.
What is the difference between myelopathy and radiculopathy in cervical spinal stenosis?
Myelopathy refers to spinal cord compression causing symptoms like difficulty walking and fine motor problems, while radiculopathy involves nerve root compression, leading to pain, numbness, and weakness in the arms.
Can cervical spinal stenosis cause problems with swallowing?
In rare cases, severe cervical spinal stenosis can cause problems with swallowing if the spinal cord compression affects the nerves that control the throat muscles.
What medications are commonly prescribed for cervical spinal stenosis?
Common medications include nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, pain relievers, and sometimes corticosteroids to reduce inflammation.
How does cervical spinal stenosis affect mobility?
It can affect mobility by causing pain, stiffness, and muscle weakness, which can make it difficult to perform daily activities and maintain balance.
What should I do if I suspect I have cervical spinal stenosis?
If you suspect you have cervical spinal stenosis, it is important to see a healthcare provider for an evaluation. Early diagnosis and treatment can help manage symptoms and prevent complications.
What is the most common age for developing cervical spinal stenosis?
Cervical spinal stenosis is most commonly seen in people over the age of 50, as it is often related to degenerative changes in the spine that occur with aging.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
