Flatback Syndrome
Flatback Syndrome occurs when the natural inward curve of the lower spine (lumbar lordosis) becomes straightened or lost. This change shifts the body’s balance forward, making it difficult to stand upright. The condition often develops after prior spine surgery, degenerative disc disease, or certain spinal disorders. Flatback Syndrome can cause back pain, fatigue, and difficulty maintaining posture. Treatment may include physical therapy, pain management, and, in some cases, surgical correction.
How Common It Is and Who Gets It? (Epidemiology)
Flatback Syndrome is relatively uncommon but is most often seen in adults who have had previous spinal fusion or scoliosis surgery. It may also occur with aging, degenerative disc disease, or conditions such as ankylosing spondylitis and osteoporosis. The risk increases with age and with previous multi-level spinal fusions that reduce normal spinal flexibility.
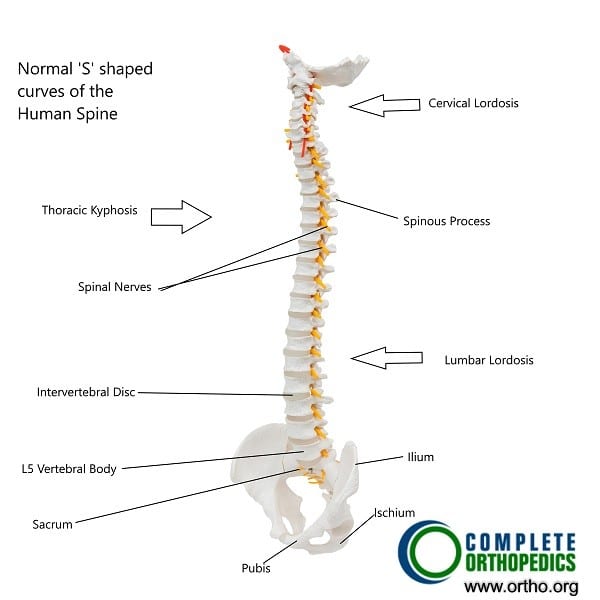
Natural curves in the human spine.
Why It Happens – Causes (Etiology and Pathophysiology)
The condition develops when the spine loses its normal lumbar curve and becomes straight. This imbalance shifts the center of gravity forward, forcing patients to bend their hips and knees to stand upright.
Common causes include:
-
Previous spinal surgery: Flatback can follow long spinal fusions for scoliosis or other deformities.
-
Degenerative disc disease: Loss of disc height reduces the natural curve.
-
Ankylosing spondylitis: A chronic inflammatory condition that fuses the spine in a flat position.
-
Osteoporosis or compression fractures: Weakened bones may collapse, altering spinal alignment.
-
Congenital deformities: Rarely, some people are born with a flat spinal shape.
How the Body Part Normally Works? (Relevant Anatomy)
The human spine has natural curves that balance the body’s weight and maintain posture. The cervical and lumbar regions curve inward (lordosis), while the thoracic spine curves outward (kyphosis). These gentle curves align the head over the pelvis, allowing easy standing and walking.
When the lumbar curve is lost, the body leans forward. To stay upright, patients unconsciously bend their hips and knees, straining muscles and joints and causing pain and fatigue.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms can vary but commonly include:
-
Difficulty standing upright: Patients often feel they are leaning forward or falling ahead of their feet.
-
Lower back pain: Caused by muscle fatigue and strain from poor balance.
-
Leg pain or heaviness: May result from nerve irritation or tight muscles.
-
Fatigue: The back and leg muscles must work harder to keep the body balanced.
-
Restricted mobility: Stiffness or limited motion in the spine.
Many patients notice worsening posture and fatigue as the day progresses. Some rely on a cane or walker for support.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a thorough review of symptoms and medical history, including prior spine surgeries. A physical examination assesses spinal alignment, gait, and flexibility.
Imaging tests help confirm the diagnosis:
-
Standing X-rays: Show overall spinal alignment and curvature.
-
CT scans: Provide detailed images of bone structure and prior surgical implants.
-
MRI: Reveals soft tissue, discs, and nerves.
These studies help identify the cause, severity, and extent of spinal imbalance.
Classification
Flatback Syndrome is often categorized by cause and severity:
-
Post-surgical: Following scoliosis or lumbar fusion surgery.
-
Degenerative: Resulting from age-related disc collapse or arthritis.
-
Inflammatory or congenital: Associated with conditions like ankylosing spondylitis or congenital deformity.
Severity is determined by how much the spinal curve and posture are altered and how much the imbalance affects walking and daily life.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other spine conditions that can mimic Flatback Syndrome include:
-
Lumbar degenerative disc disease
-
Kyphosis (forward rounding of the spine)
-
Spondylolisthesis (slipped vertebra)
-
Muscle weakness or imbalance
-
Hip or knee arthritis affecting posture
Treatment Options
Non-Surgical Care
Initial treatment focuses on relieving pain, improving posture, and restoring flexibility.
-
Physical therapy: Strengthening core and back muscles, stretching, and gait training.
-
Pain medication: NSAIDs or acetaminophen to reduce inflammation and discomfort.
-
Heat or cold therapy: Helps ease muscle tension.
-
Injections: Epidural or nerve-block injections may provide temporary pain relief.
-
Lifestyle changes: Weight management and posture correction during daily activities.
Surgical Care
Surgery may be recommended when conservative care fails or if spinal imbalance severely limits mobility.
Common procedures include:
-
Spinal fusion revision: Restores the normal spinal curve by correcting or extending previous fusions.
-
Osteotomy: A wedge-shaped section of bone is removed to realign the spine and restore balance.
-
Decompression surgery: Removes bone or disc tissue pressing on nerves.
These surgeries often use screws, rods, or cages to stabilize the corrected spine. Recovery times vary, but most patients experience significant improvement in posture and pain after surgery.
Recovery and What to Expect After Treatment
-
Conservative care: Improvement may occur within weeks to months with consistent therapy and posture training.
-
After surgery: Patients usually stay in the hospital for several days. Rehabilitation includes physical therapy to regain strength and improve balance. Full recovery can take several months.
Most patients report improved posture, reduced pain, and greater mobility following successful treatment.
Possible Risks or Side Effects (Complications)
As with any spinal procedure, possible complications include:
-
Infection or bleeding
-
Nerve injury or weakness
-
Failure of bone fusion or implant issues
-
Persistent pain or stiffness
-
Blood clots or anesthesia risks
Proper surgical planning and rehabilitation minimize these risks.
Long-Term Outlook (Prognosis)
With appropriate treatment, most patients regain balance and mobility. Physical therapy and posture training help maintain long-term results. Surgical correction can provide lasting relief when conservative care is not enough, though ongoing spine monitoring is important to prevent recurrence or complications.
Out-of-Pocket Costs
Medicare
CPT Code 22612 – Posterior Spinal Fusion (Lumbar): $382.85
CPT Code 22207 – Osteotomy (for Deformity Correction): $580.50
CPT Code 63300 – Vertebral Column Resection: $450.25
CPT Code 22842 – Segmental Instrumentation (3–6 Segments): $185.26
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible has been met. The remaining 20% coinsurance is typically the patient’s responsibility. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield are designed to cover this 20%, significantly reducing or eliminating any out-of-pocket expenses for Medicare-approved spine surgeries. These supplemental plans work seamlessly with Medicare to ensure patients receive comprehensive coverage for complex reconstructive procedures like deformity correction and spinal stabilization.
If you have a secondary insurance plan—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare has processed the claim. After your deductible is satisfied, the secondary plan can cover remaining balances, including coinsurance or non-covered costs. Most secondary insurance plans include a small deductible, typically ranging between $100 and $300, depending on the specific policy and whether the procedure is performed at an in-network facility.
Workers’ Compensation
If your spinal deformity or instability resulted from a work-related injury or repetitive strain, Workers’ Compensation will fully cover all surgical costs, including osteotomy, fusion, instrumentation, and resection procedures. You will not have any out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your spinal deformity or instability is the result of an automobile accident, No-Fault Insurance will pay for all medically necessary surgical procedures, such as spinal fusion, osteotomy, or instrumentation. You may only be responsible for a small deductible depending on your insurance policy terms.
Example
Anthony, a 67-year-old patient, required lumbar deformity correction involving a spinal fusion (CPT 22612), osteotomy (CPT 22207), and segmental instrumentation (CPT 22842). His estimated Medicare out-of-pocket costs were $382.85, $580.50, and $185.26. Because he had supplemental insurance through Blue Cross Blue Shield, the remaining 20% coinsurance was fully covered, resulting in no out-of-pocket expense for his surgery.
Frequently Asked Questions (FAQ)
Q. Can Flatback Syndrome improve without surgery?
A. Mild cases can often be managed with physical therapy, pain relief, and posture training.
Q. Is Flatback Syndrome permanent?
A. Without correction, the loss of curvature can persist, but symptoms can be managed effectively.
Q. Will surgery restore normal posture?
A. In most cases, surgery can significantly improve alignment and allow patients to stand upright comfortably.
Q. How long is recovery after surgery?
A. Most patients recover within 3–6 months, with ongoing physical therapy for balance and strength.
Summary and Takeaway
Flatback Syndrome occurs when the normal curve of the lower spine straightens, causing pain and difficulty standing upright. It may follow spinal surgery, arthritis, or age-related degeneration. Treatment includes therapy, medication, and, when needed, surgical correction. With early diagnosis and proper management, patients can regain comfort, posture, and mobility.
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is managed by orthopedic spine surgeons and neurosurgeons, with support from physical therapists, pain specialists, and rehabilitation teams.
When to See a Specialist?
You should see a specialist if you have:
-
Persistent back pain that worsens with standing or walking
-
Trouble standing upright or maintaining balance
-
Increasing fatigue or difficulty performing daily activities
When to Go to the Emergency Room?
Seek immediate care if you experience:
-
Sudden loss of strength or sensation in the legs
-
Severe back pain with numbness or bladder/bowel changes
-
Inability to walk due to pain or instability
What Recovery Really Looks Like?
Recovery is gradual. After therapy or surgery, patients regain posture and comfort over several months. Consistent physical therapy and regular follow-up imaging ensure stable, lasting results.
What Happens If You Ignore It?
Without treatment, the forward tilt may worsen, causing chronic pain, spinal fatigue, and mobility issues. Over time, severe deformity may make walking or standing nearly impossible.
How to Prevent It?
-
Maintain good posture and core strength.
-
Engage in low-impact exercise such as swimming or yoga.
-
Avoid repetitive heavy lifting.
-
Treat osteoporosis or arthritis early to prevent spine collapse.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and protein supports bone strength. Avoid smoking and excessive alcohol, which can weaken bone tissue and slow recovery.
Activity and Lifestyle Modifications
After recovery, stay active with gentle, spine-friendly activities. Maintain an ergonomic workstation, practice proper lifting techniques, and attend regular checkups to monitor spinal alignment.
Do you have more questions?
What is flatback syndrome?
Flatback syndrome is a condition where the natural inward curve of the lower spine (lordosis) is lost, resulting in a spine that appears flat and causing a forward-leaning posture.
What are the symptoms of flatback syndrome?
Symptoms include difficulty standing upright, lower back pain, fatigue, pain in the legs, and restricted mobility.
What causes flatback syndrome?
It can be caused by degenerative disc disease, previous spinal surgeries (especially spinal fusions), conditions like Scheuermann’s kyphosis or ankylosing spondylitis, and poor posture over time.
When is surgery necessary for flatback syndrome?
Surgery may be necessary if non-surgical treatments fail to relieve symptoms, if there is significant spinal deformity, or if there is nerve compression causing severe pain or functional impairment.
What are the non-surgical treatment options for flatback syndrome?
Non-surgical treatments include physical therapy, pain management with medications, and sometimes wearing a brace to support the spine.
What surgical options are available for flatback syndrome?
Surgical options include spinal fusion revision, osteotomy (removal of a bone section to correct alignment), and decompression surgery to relieve nerve pressure.
Can flatback syndrome be prevented?
While not all cases can be prevented, maintaining good posture, staying active, managing weight, and avoiding unnecessary spinal surgeries can reduce the risk.
Can flatback syndrome worsen over time?
Yes, without appropriate treatment and management, the condition can worsen, leading to increased pain and disability.
Is flatback syndrome common?
It is relatively uncommon, often seen as a complication of previous spinal surgeries or specific spinal conditions.
How effective is physical therapy for flatback syndrome?
Physical therapy can be very effective in strengthening the muscles that support the spine, improving posture, and reducing pain.
Are there any risks associated with surgery for flatback syndrome?
As with any surgery, risks include infection, bleeding, nerve damage, and complications related to anesthesia. There is also a risk of the surgery not fully correcting the deformity or relieving symptoms.
What types of exercises are recommended for flatback syndrome?
Core strengthening exercises, stretching, and activities that promote good posture are recommended.
How long is the recovery period after surgery for flatback syndrome?
Recovery can take several months. The initial hospital stay might be a few days to a week, followed by a period of rehabilitation and gradual return to normal activities.
What is the prognosis for someone with flatback syndrome?
With appropriate treatment, many people can manage their symptoms effectively and maintain a good quality of life. Surgical correction can significantly improve posture and reduce pain.
Can flatback syndrome lead to other health problems?
If left untreated, it can lead to chronic pain, reduced mobility, and an increased risk of falls and other injuries due to the altered posture.
Can flatback syndrome recur after treatment?
Recurrence is possible, especially if the underlying causes are not fully addressed or if there is degeneration in other parts of the spine.
Can children develop flatback syndrome?
It is more common in adults, especially those with a history of spinal surgery or specific spinal conditions. However, children with conditions like Scheuermann’s kyphosis could potentially develop it.
Is flatback syndrome the same as scoliosis?
No, scoliosis involves a sideways curvature of the spine, whereas flatback syndrome involves a loss of the normal inward curvature of the lower spine.
How does flatback syndrome affect daily activities?
It can make standing and walking for long periods difficult, cause chronic pain, and lead to fatigue, impacting overall mobility and quality of life.
What lifestyle changes can help manage flatback syndrome?
Maintaining a healthy weight, staying active with appropriate exercises, using proper posture, and following a treatment plan can help manage symptoms.
Are there any supportive devices that can help with flatback syndrome?
Braces can sometimes be used to support the spine and improve posture. Additionally, ergonomic furniture and supportive shoes can help reduce strain.
How does flatback syndrome affect sleep?
Chronic pain and discomfort can interfere with sleep. Finding a comfortable sleeping position and using supportive mattresses and pillows can help improve sleep quality.
What role do diet and nutrition play in managing flatback syndrome?
A balanced diet that supports overall health, including bone and muscle health, can be beneficial. Maintaining a healthy weight is particularly important to reduce strain on the spine.
Can alternative therapies help with flatback syndrome?
Some individuals find relief through alternative therapies like chiropractic care, acupuncture, or massage, but these should be used in conjunction with conventional treatments and under the guidance of a healthcare professional.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
