Transforaminal Lumbar Interbody Fusion Surgery
Transforaminal lumbar interbody fusion surgery (TLIF) is a widely used surgical procedure aimed at spinal stabilization and decompression. It is performed to treat various lumbar spine conditions, including degenerative disc disease, spondylolisthesis, and failed back surgery syndrome. By fusing two adjacent vertebrae, TLIF restores stability to the spine and alleviates symptoms of pain and nerve compression.
Functional Anatomy
The lumbar spine consists of five vertebrae that support much of the body’s weight and are critical for movement. The intervertebral discs between the vertebrae act as cushions, absorbing shock and allowing for movement. When a herniated disc or degenerative disease compresses the spinal nerves, it can cause radiculopathy (nerve pain radiating to the legs), often treated with spinal fusion surgery like TLIF.
TLIF involves removing the damaged disc material, decompressing the affected nerves, and inserting a bone graft or spinal cage to restore disc height and support vertebral stability. The procedure uses a transforaminal (side-entry) approach to access the spine without damaging back muscles.
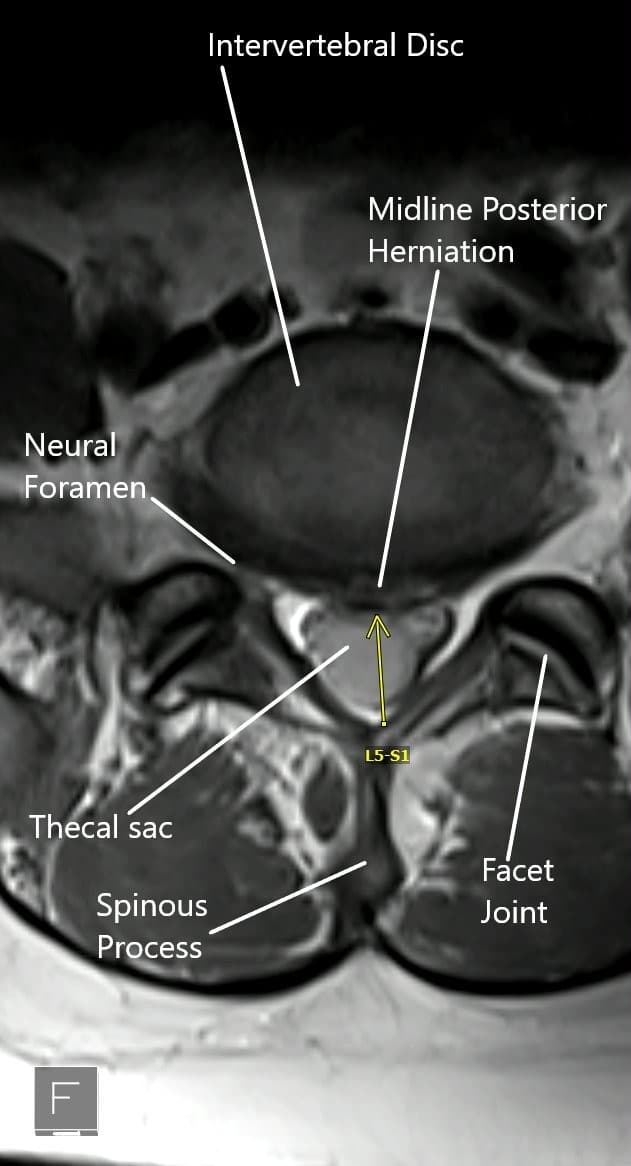
MRI of the lumbar spine in axial view showing central disc herniation.
Biomechanics or Physiology
TLIF surgery restores proper spinal alignment and relieves pressure on the spinal nerves, which reduces pain and restores function. The bone graft or cage inserted between the vertebrae provides a scaffold for bone fusion, allowing the vertebrae to heal together into a solid, stable structure. Pedicle screws and rods are then used to stabilize the vertebrae during the healing process.
The transforaminal approach allows access to the spine through the side, which minimizes damage to muscles and other soft tissues, leading to less postoperative pain and quicker recovery.
Common Variants and Anomalies
While TLIF is effective for many patients with degenerative lumbar conditions, some anatomical factors may affect the approach. For example, previous spine surgeries may create scar tissue that complicates access to the spine. Multilevel disease or extensive disc involvement may also limit the suitability of TLIF, as the procedure typically targets one side of the disc.
Patients with metabolic bone disorders, such as osteoporosis, may have an increased risk of nonunion or complications due to the reduced ability of their bones to fuse.
Clinical Relevance
TLIF is particularly beneficial for patients with degenerative spine conditions, including spondylolisthesis, where one vertebra slips over another, or failed back surgery syndrome, where previous spine surgery has not provided relief. The goal of TLIF is not only to provide pain relief but also to restore stability and prevent further degeneration of the spine.
TLIF is a minimally invasive procedure compared to traditional spinal fusion techniques. It provides significant benefits in terms of reduced muscle trauma, shorter recovery times, and improved postoperative outcomes.
Imaging Overview
Imaging techniques such as X-rays, MRI, and CT scans are critical in diagnosing lumbar spine issues and determining the appropriate level for surgery. For TLIF, preoperative imaging is used to identify the degree of disc degeneration, nerve compression, and the alignment of the spine. During the surgery, fluoroscopy is often used to guide the placement of screws and the insertion of the bone graft or spinal cage.
Associated Conditions
Conditions that may be treated with TLIF include:
-
Degenerative disc disease – wear and tear of spinal discs, leading to nerve compression and pain.
-
Spondylolisthesis – slippage of one vertebra over another, often due to degeneration or injury.
-
Failed back surgery syndrome – persistent pain after previous spine surgery.
-
Spinal canal stenosis – narrowing of the spinal canal, causing nerve compression.
-
Herniated discs – protrusion of disc material, compressing spinal nerves.
TLIF is effective in treating these conditions by decompressing the spinal cord or nerves and stabilizing the spine.
Surgical or Diagnostic Applications
TLIF is used when conservative treatments such as physical therapy, medication, and injections fail to provide adequate relief. Discectomy, which involves removing the herniated disc material, is often combined with the fusion procedure to restore stability.
The transforaminal approach allows access to the lumbar spine without requiring large incisions or significant muscle disruption. Pedicle screws and rods provide spinal stability, while a bone graft or spinal cage is inserted to promote fusion between the vertebrae.
Transforaminal Lumbar Interbody Fusion Surgery Indications
Lumbar fusion surgery is performed after all conservative management options have been tried without satisfactory results. Various conditions that may be treated with fusion surgery are:-
- Degenerative disk disease may cause symptoms of back pain and radiculopathy. With advancing age, there may be a loss of disk height resulting in subsequent segment instability. The body tries to re-align by enlargement of ligaments and bony structures that may impinge upon the neural structures.
- Recurrent intervertebral disc herniations may result after traumatic events or degenerative conditions. The herniated disk may compress the exiting or traversing nerve roots causing symptoms of radiculopathy.
- Spondylolisthesis occurs as a result of misplaced vertebrae due to developmental, isthmic, or degenerative causes. The displaced vertebrae may cause back pain and symptoms of radiculopathy or neurogenic compression.
- Spinal canal stenosis occurs as a result of narrowing of the vertebral canal or the neural foramen.
- Failed back surgery involves the continuation of symptoms of back pain or radiculopathy after prior spine surgery. The failure of surgery may be due to implant failure, adjacent level degeneration, wrong diagnosis, incomplete surgery, etc.
TLIF Procedure
The surgery is performed under general anesthesia, and the patient is placed on his/her abdomen. The surgeon gives a skin incision slightly towards the body’s side (about 4cm from the midline) over the involved segment. A metallic wire is passed under fluoroscopic guidance towards the facet joint complex.
Serial dilators are passed over the wire to create a muscle splitting rather than cutting exposure. The tubular retractors are then used to visualize the involved segment.
The surgeon then decompresses the segment by removing the facet joint and by performing laminectomy. The intervertebral disk material is removed from the involved side. Any other tissue compressing upon the neural tissue is removed.
The surgeon then introduces a cage between the involved vertebrae after the endplate preparation. The cage may be made of metal alloy or high-grade plastic such as PEEK (poly ether-ether ketone). The bone cage functions to maintain the disc space between the two vertebrae.
The bone cage is filled with bone graft material. The bone graft may be taken from the patient’s pelvis during the surgery or maybe utilized from a bone bank. The bone graft ensures speedy union between the vertebrae.
Mirror incisions are made on the other side to introduce pedicle screws. Rods are tightened over the pedicle screws to support the arthrodesis in the front. The screw and rod construct also decompress the vertebrae by distraction.
Throughout the surgery, care is taken to protect the nerve roots and the dural sac from inadvertent damage. The incisions are closed in layers, and the patients may go home after a day’s stay at the hospital or may go home the same day if a minimally invasive technique is used.
Transforaminal Lumbar Interbody Fusion Surgery Complications
Although the risk of complications remains relatively low, there may be potential complications of infection, blood loss, nonunion of the fusion, implant failure, blood clots, etc. The operating surgeon will discuss all the potential risks and complications with the patient before the surgery.
Transforaminal Lumbar Interbody Fusion Surgery Postoperative Care
The majority of the patients are advised to walk the next day of the surgery and resume their daily activities. They are advised against the lifting of heavyweights and sudden bending or twisting movements. Physical therapy is initiated to strengthen the back muscles and improve flexibility. Pain medications may be used in the initial postoperative period.
Benefits of TLIF
The transforaminal approach utilized the entry from the side of the back. The entry prevents cutting of the back muscles to reach the involved segment. The muscles and other soft tissues are instead separated with the use of tubular dilators. This has been shown to improve the postoperative recovery period.
Patients treated with the TLIF approach experience less postoperative pain and require fewer doses of pain medications. They can also participate in physical therapy earlier than the patients treated with the traditional posterior approach.
A large amount of bone graft can be placed from the side of the spine that ensures a steadier fusion. The retraction of the dural sac and the nerve roots is minimum, so the chances of nerve injury and dural tear are far less with the transforaminal approach.
The lateral trajectory used in the transforaminal approach can also be used in patients with prior spine surgery. The approach may be used in patients with far lateral disc herniations and instability.
Contraindications
The transforaminal approach is contraindicated in patients with metabolic bone disorders such as osteoporosis. The TLIF surgery is also not indicated in patients with disc infection, multilevel disease, extensive scarring from prior surgery. The approach is also not indicated in patients with complete disc involvement as through TLIF, the surgeon can reach only one side of the disc.
Prevention and Maintenance
After TLIF surgery, patients are advised to follow a comprehensive rehabilitation plan that includes physical therapy to strengthen the muscles around the spine and improve flexibility. This reduces the likelihood of complications and helps to prevent future episodes of back pain. Maintaining proper posture, avoiding heavy lifting, and engaging in regular exercise are also recommended for long-term spinal health.
Patients should also monitor bone health and manage metabolic bone conditions such as osteoporosis to ensure successful fusion and prevent complications like nonunion.
Research Spotlight
A recent study compared the biportal endoscopic transforaminal lumbar interbody fusion (TLIF) technique with traditional TLIF for treating degenerative lumbar conditions. The study highlighted that biportal endoscopic TLIF, a minimally invasive approach, offers benefits such as reduced muscle trauma, less postoperative pain, and quicker recovery compared to the conventional method.
The procedure involves using two small incisions and specialized tools to clear the intervertebral disc and insert a bone graft and cage, stabilizing the segment. Outcomes from the study indicate that this approach provides similar clinical and radiological results to traditional surgery but with less disruption to surrounding tissues, leading to shorter recovery times and improved postoperative mobility.
These findings suggest that biportal endoscopic TLIF could be a promising alternative for patients with lumbar degenerative diseases (“Study on biportal endoscopic TLIF for lumbar degenerative diseases – See PubMed“).
Summary and Key Takeaways
Transforaminal lumbar interbody fusion surgery (TLIF) is an effective, minimally invasive technique used to treat various degenerative lumbar spine conditions, such as degenerative disc disease, spondylolisthesis, and failed back surgery syndrome. By stabilizing the spine and relieving pressure on the nerves, TLIF offers significant pain relief and improves function.
The transforaminal approach minimizes muscle disruption, leading to faster recovery and less postoperative pain compared to traditional methods. Pedicle screws and rods provide spinal stability, while bone grafts or spinal cages promote fusion between the vertebrae.
While TLIF is effective for many patients, it may not be suitable for individuals with metabolic bone disorders, multilevel spine disease, or extensive scarring from prior surgeries. It is essential for patients to consult with their healthcare provider to determine if TLIF is the right option based on their specific condition.
Do you have more questions?
What is the main goal of TLIF surgery?
The primary goal of TLIF surgery is to stabilize the spine and promote the fusion of vertebrae by reducing painful motion in the affected spinal segment, which helps relieve chronic pain caused by conditions such as degenerative disc disease or spondylolisthesis.
Who is a good candidate for TLIF?
Ideal candidates are individuals with chronic lower back pain or leg pain due to conditions like degenerative disc disease, spinal stenosis, or spondylolisthesis that have not responded to conservative treatments such as physical therapy or medication.
How is TLIF different from other spinal fusion surgeries like PLIF or ALIF?
TLIF uses a more lateral approach to access the disc space, reducing the need for nerve retraction compared to posterior lumbar interbody fusion (PLIF). Unlike anterior lumbar interbody fusion (ALIF), which requires an additional incision in the abdomen, TLIF achieves fusion through a single posterior incision.
Is TLIF a minimally invasive surgery?
TLIF can be performed as a traditional open procedure or using minimally invasive techniques. Minimally invasive TLIF involves smaller incisions, less muscle dissection, and a quicker recovery period, but the technique chosen depends on the patient’s specific condition.
What materials are used for the bone graft in TLIF?
Bone graft materials may include autograft (your own bone, typically from the iliac crest), allograft (donor bone), or synthetic bone substitutes. The choice depends on the patient’s situation and surgeon’s preference.
How long does the TLIF surgery take?
The length of the procedure varies based on the number of levels fused and whether it’s performed minimally invasively, but on average, TLIF takes about 2-4 hours.
What are the risks or complications associated with TLIF?
While TLIF is generally safe, potential complications include infection, nerve injury, blood clots, nonunion (failure of the bones to fuse), hardware failure, and persistent pain. However, many of these risks are minimized with proper surgical technique and post-operative care.
How much pain will I have after TLIF surgery?
While pain is expected in the immediate post-operative period, it is usually managed with medication. Most patients experience a reduction in their chronic back or leg pain over time as the spine stabilizes.
How soon after TLIF surgery can I walk?
Most patients are encouraged to start walking as early as the day after surgery or within 48 hours, depending on their comfort level and surgical outcome.
What kind of anesthesia is used for TLIF?
General anesthesia is typically used for TLIF surgery, meaning the patient will be completely unconscious during the procedure.
How long is the hospital stay after TLIF?
Patients typically stay in the hospital for 3 to 7 days after surgery, depending on their health condition and recovery progress.
Will I need a brace after TLIF surgery?
In some cases, a lumbar brace may be recommended to support the spine during the early stages of recovery, especially if significant bone loss or osteoporosis is present.
When can I return to work after TLIF?
This depends on the type of work you do. Patients with desk jobs may return to work within 4-6 weeks, while those with physically demanding jobs may need 3-6 months before returning to full activity.
What are the signs that the bone fusion was successful?
Successful fusion is usually confirmed through follow-up X-rays or CT scans showing solid bone formation between the vertebrae. Clinically, a reduction in pain and improved mobility are good indicators.
What happens if the bones don’t fuse properly after TLIF?
This is known as nonunion or pseudoarthrosis. In these cases, further treatment may involve bone stimulators, revision surgery, or other interventions to promote fusion.
Can TLIF be performed on multiple spinal levels?
Yes, TLIF can be performed on multiple levels if necessary, though it increases the complexity and length of the surgery.
Will I need physical therapy after TLIF surgery?
Yes, physical therapy is often an essential part of the recovery process. It helps strengthen the muscles around the spine, restore flexibility, and improve overall function.
Is TLIF effective for treating leg pain (sciatica)?
Yes, TLIF can be very effective for treating leg pain caused by nerve root compression, such as sciatica, by relieving pressure on the nerves and stabilizing the affected segment.
How long will it take to fully recover from TLIF?
Full recovery can take 6-12 months as the fusion progresses. During this period, patients will gradually return to their normal activities, guided by physical therapy and follow-up assessments.
What is the long-term success rate of TLIF surgery?
Studies indicate that 85-95% of patients achieve solid fusion and significant pain relief after TLIF. Long-term outcomes depend on factors such as patient compliance with post-operative care and avoidance of smoking, which impairs bone healing.
Is it safe to undergo TLIF if I’ve had previous spine surgery?
Yes, TLIF is often preferred for patients with previous spine surgery, as its lateral approach allows the surgeon to avoid areas of scar tissue that could complicate other fusion techniques.
What can I do to improve my chances of a successful outcome?
To improve your chances of success, it is crucial to follow your surgeon’s instructions closely. Avoid smoking, maintain a healthy diet rich in calcium and vitamin D, and participate in physical therapy as recommended.
Will I be able to resume sports or physical activities after TLIF?
Most patients can return to low-impact activities, such as walking or swimming, within 6-8 weeks. Higher-impact sports, like running or weightlifting, may take longer—up to 6-12 months—but should only be resumed after your surgeon gives clearance.
Will the hardware (screws and rods) need to be removed later?
In most cases, the hardware used in TLIF is permanent and does not need to be removed. However, in rare instances where the hardware causes discomfort or complications, removal may be considered after fusion is confirmed.
Can TLIF correct spinal deformities like scoliosis?
TLIF can be used to treat certain spinal deformities, such as spondylolisthesis or mild scoliosis, by realigning and stabilizing the spine. However, severe scoliosis may require more complex procedures.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
