Diagnosis of Sciatica
Sciatica refers to pain that travels from the lower back or buttock down into the leg, caused by compression or irritation of the sciatic nerve or its roots (L4–S3). The pain may be sharp, burning, or shooting and is often accompanied by numbness, tingling, or weakness in the affected leg.
Most cases of sciatica result from a herniated disc, spinal stenosis, or degenerative changes in the lower spine. In most patients, symptoms improve with rest, medications, and physical therapy, but accurate diagnosis is essential for effective treatment.
How Common It Is and Who Gets It? (Epidemiology)
Sciatica affects approximately 10–40% of adults at some point in their lives. It is most common in adults aged 30–60 years, especially those with physically demanding jobs or sedentary lifestyles. Risk factors include poor posture, obesity, smoking, and repetitive spinal stress.
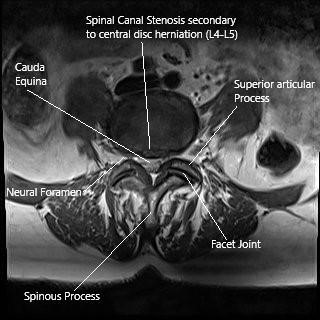
MRI of the Lumbar spine in axial section central disc herniation.
Why It Happens – Causes (Etiology and Pathophysiology)
Sciatica occurs when one or more of the spinal nerve roots forming the sciatic nerve become compressed or inflamed. Common causes include:
-
Lumbar disc herniation: The soft inner portion of a spinal disc bulges or ruptures, pressing on a nerve root.
-
Spinal stenosis: Narrowing of the spinal canal compresses the nerves.
-
Degenerative disc disease: Age-related disc wear leads to instability and inflammation.
-
Spondylolisthesis: One vertebra slips forward over another.
-
Tumors or infections: Rare but serious causes of nerve irritation.
How the Body Part Normally Works? (Relevant Anatomy)
The sciatic nerve is the largest nerve in the body, formed by the fusion of nerve roots from L4 to S3 in the lower spine. It runs from the lower back through the buttocks and down the back of each leg.
When one of the nerve roots is irritated or compressed, pain signals are transmitted along the nerve, producing the characteristic symptoms of sciatica.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of sciatica may include:
-
Sharp, burning, or shooting pain radiating from the back or buttock into the leg.
-
Pain worse than the backache itself, often felt below the knee.
-
Numbness or tingling in the leg or foot.
-
Weakness in the lower extremity.
-
Pain aggravated by sitting, coughing, sneezing, or straining.
-
Difficulty walking or standing for long periods.
When caused by spinal stenosis, symptoms may worsen when walking downhill or standing upright and improve when sitting or bending forward.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis of sciatica begins with a detailed medical history and a physical examination. Imaging is not always necessary at first, as most cases improve within a few weeks of conservative care.
History
Your doctor will ask questions such as:
-
Where do you feel the pain?
-
When did it start, and was it sudden or gradual?
-
Does sitting, coughing, or walking worsen it?
-
Is there tingling, numbness, or weakness in the leg?
-
Do you have bladder or bowel control problems?
-
Have you noticed any weight loss, fever, or trauma?
Pain due to a herniated disc typically worsens with sitting or bending, while pain from spinal stenosis is aggravated by walking or standing and relieved by sitting or leaning forward.
Physical Examination
The physician will perform a complete neurological exam to assess nerve function and identify the affected root.
-
Muscle strength: Tested by walking on toes (S1), heels (L5), or bending the knee (L4).
-
Reflexes:
-
Decreased patellar reflex suggests L4 involvement.
-
Diminished Achilles reflex indicates S1 involvement.
-
-
Sensory testing: Checks sensation in the thighs, calves, and feet.
-
Straight leg raise (SLR) test: Pain during leg elevation indicates nerve root irritation.
-
Gait assessment: Identifies weakness or imbalance when walking.
These findings help pinpoint which nerve root is compressed.
Imaging
Imaging is used when symptoms persist beyond 6–12 weeks or if red-flag symptoms appear (such as bowel or bladder loss).
-
X-rays: Detect fractures, alignment issues, or bone spurs.
-
CT scan: Provides detailed views of the spine’s bone structure; sometimes used with a dye (CT myelogram) for better visualization.
-
MRI: The gold standard for diagnosing disc herniation, nerve compression, or soft tissue abnormalities.
-
Electromyography (EMG): Evaluates electrical activity in muscles and helps locate the level of nerve compression.
Classification
Sciatica is classified by duration and underlying cause:
-
Acute: Lasts less than 6 weeks.
-
Chronic: Persists for more than 3 months.
It can also be categorized by the involved nerve root (L4, L5, or S1).
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Hip or sacroiliac joint dysfunction
-
Peripheral neuropathy (often due to diabetes)
-
Piriformis syndrome
-
Vascular claudication (poor leg circulation)
-
Tumors or infections
Treatment Options
Non-Surgical Care
Most cases of sciatica resolve with conservative treatment:
-
Medications: NSAIDs, muscle relaxants, and short-term corticosteroids.
-
Physical therapy: Core strengthening, stretching, and posture correction.
-
Heat or ice therapy: Reduces inflammation and muscle spasm.
-
Activity modification: Avoid prolonged sitting and heavy lifting.
-
Epidural steroid injections: Reduce inflammation and nerve irritation for persistent cases.
Surgical Care
Surgery is considered for patients with:
-
Severe or progressive neurological deficits.
-
Persistent pain despite 6–12 weeks of conservative therapy.
-
Loss of bladder or bowel control (a surgical emergency).
Common procedures include: -
Microdiscectomy: Removal of herniated disc material compressing the nerve.
-
Laminectomy: Decompression of the spinal canal in stenosis cases.
Recovery and What to Expect After Treatment
-
Conservative management: Most patients recover within 4–6 weeks.
-
After surgery: Patients usually walk the next day, with full recovery in 4–8 weeks.
Regular physical therapy and ergonomic modifications help prevent recurrence.
Possible Risks or Side Effects (Complications)
-
Persistent or recurrent pain.
-
Nerve damage causing weakness or numbness.
-
Bowel or bladder dysfunction if compression persists.
-
Surgical complications (infection, scar tissue formation).
Long-Term Outlook (Prognosis)
The prognosis for sciatica is excellent. About 90% of patients improve without surgery. For those who require surgery, modern techniques provide lasting pain relief and functional recovery.
Out-of-Pocket Costs
Medicare
CPT Code 63030 – Discectomy (Removal of Herniated Disc): $225.06
CPT Code 63047 – Laminectomy (Decompression): $271.76
CPT Code 22612 – Fusion (Posterior Lumbar): $382.85
CPT Code 22630 – Interbody Fusion (PLIF/TLIF): $387.42
CPT Code 22842 – Instrumentation (Rods, Screws, Plates – 3–6 Segments): $185.26
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually cover this remaining 20%, meaning most patients have little to no out-of-pocket cost for Medicare-approved spine surgeries. These supplemental plans coordinate directly with Medicare to ensure comprehensive coverage for procedures like decompression, fusion, and stabilization performed for sciatica.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare has processed the claim. After the deductible is satisfied, secondary insurance can cover any remaining coinsurance or balance. Deductibles for these plans generally range between $100 and $300, depending on your policy and whether the procedure is performed in-network.
Workers’ Compensation
If your sciatica developed or worsened due to a work-related injury, Workers’ Compensation will cover the entire cost of medical and surgical care, including discectomy, laminectomy, or spinal fusion if required. You will not have any out-of-pocket expenses for approved services under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your sciatica resulted from a motor vehicle accident, No-Fault Insurance will pay for all necessary diagnostic, surgical, and hospital expenses. This includes decompression, fusion, or instrumentation if medically required. The only potential charge would be a small deductible depending on your specific policy terms.
Example
David, a 60-year-old patient, suffered from severe sciatica due to a herniated lumbar disc and underwent discectomy (CPT 63030) and posterior fusion (CPT 22612). His Medicare out-of-pocket costs were $225.06 and $382.85. Since he had supplemental insurance through Blue Cross Blue Shield, the remaining 20% not paid by Medicare was fully covered, leaving him with no out-of-pocket expense for his surgery.
Frequently Asked Questions (FAQ)
Q. How is sciatica diagnosed?
A. Diagnosis is based on your symptoms, physical examination, and, if needed, imaging studies such as an MRI to confirm nerve compression.
Q. Do I need an MRI for sciatica?
A. Not always. Most cases improve with conservative care, and imaging is reserved for persistent or worsening symptoms.
Q. How do doctors identify which nerve is affected?
A. Through neurological tests that evaluate muscle strength, reflexes, and sensation in the legs, along with special maneuvers like the straight leg raise test.
Q. When should I see a doctor for sciatica?
A. Seek medical care if you have pain lasting more than a few weeks, pain that radiates below the knee, or weakness, numbness, or bladder/bowel changes.
Summary and Takeaway
Sciatica is pain radiating from the lower back into the leg, caused by irritation or compression of the sciatic nerve. Diagnosis is primarily clinical, supported by imaging when necessary. Most cases improve with conservative care, but timely evaluation and treatment prevent long-term nerve damage and restore full function.
Clinical Insight & Recent Findings
A recent observational study compared outcomes of early versus delayed microdiscectomy in patients with sciatica caused by lumbar disc herniation. The study followed 237 patients who underwent surgery and divided them into two groups based on symptom duration: early surgery (<6 months) and delayed surgery (≥6 months).
Results showed that early surgery led to significantly greater pain relief and functional improvement at 1 to 3 months postoperatively, with lower Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) scores compared to delayed surgery. However, by 12 months, the differences between the groups had diminished, and long-term outcomes were comparable. Complication rates were similar (5.7% vs. 5.2%), indicating that early intervention does not increase surgical risk.
The authors concluded that performing lumbar decompression surgery within six months after failed conservative treatment yields faster recovery, improved short-term outcomes, and reduced dependence on opioids. These findings support early surgical management when conservative therapy is ineffective. (Study of early versus delayed surgery for sciatica – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Sciatica is diagnosed and treated by orthopedic spine surgeons, neurosurgeons, pain management specialists, and physical therapists working together to create individualized treatment plans.
When to See a Specialist?
You should see a specialist if you experience:
-
Persistent leg pain for more than 2 weeks.
-
Numbness or tingling in the foot or toes.
-
Weakness when lifting the foot (foot drop).
-
Difficulty walking or standing for long periods.
When to Go to the Emergency Room?
Seek immediate care if you develop:
-
Loss of bladder or bowel control.
-
Severe, worsening leg weakness.
-
Numbness in the groin or saddle area.
What Recovery Really Looks Like?
Most patients recover gradually over 4–6 weeks. Pain subsides first, followed by improvement in strength and flexibility. For surgical patients, physical therapy aids faster recovery and prevents recurrence.
What Happens If You Ignore It?
Untreated sciatica can lead to chronic pain, persistent weakness, or permanent nerve damage. Early treatment ensures faster recovery and better long-term results.
How to Prevent It?
-
Practice good posture when sitting and standing.
-
Exercise regularly to strengthen back and core muscles.
-
Use proper lifting techniques.
-
Maintain a healthy weight.
-
Avoid prolonged sitting.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and omega-3 fatty acids supports bone and joint health. Staying hydrated maintains spinal disc elasticity and nerve function.
Activity and Lifestyle Modifications
Engage in low-impact exercises such as walking, swimming, and stretching. Avoid prolonged sitting or heavy lifting, and maintain a healthy body weight to reduce stress on the spine.
Do you have more questions?
Can sciatica cause knee pain?
Sciatica pain is usually radiated along the back or the side of the thigh and knee into the leg. Occasionally, patients may present with a confusing picture of knee problem, but maybe having sciatica. A thorough history and examination by the physician as well as diagnostic tests in the form of x-rays and MRI may be needed to confirm the diagnosis.
How to fix sciatica nerve pain?
Sciatica nerve pain can be relieved to various modalities. To start with, antiinflammatory medications like ibuprofen, naproxen or Tylenol may help. If pain is not relieved with the medications, physical therapy, chiropractor and acupuncture may also help. The patient may also take medications including gabapentin or pregabalin for pain relief.
The patient should take a short period of bed rest for a day or two. The patient should continue to do normal usual activities. If the pain is not relieved, he should see his doctor. Epidural injection or nerve root blocks may help in relieving the sciatica pain. Patients who are not having any relief with any of the above-mentioned treatment plans, may need an MRI for confirmation of diagnosis and possibly surgery to relieve their pain.
How do you diagnose sciatica?
Sciatica is a clinical diagnosis, which can be corroborated by imagings with or without nerve conduction/EMG studies. Typical patient will present with pain radiating down one leg along the back or the side of the thigh index. They may have been associated with tingling and numbness or back pain.
Occasionally, patients may have weakness in the toes or the ankle. Once the clinical diagnosis is made, confirmation can be done using x-rays and MRI. In patients who have a confusing picture due to underlying comorbidity or atypical presentation, nerve conduction study and electromyographic study can be done to further confirm or rule out sciatica.
Is heat or ice better for sciatica?
Heat is usually better in patients who have sciatica, though patients who are not relieved with heat should also try ice or occasionally rhythmic use of heat and ice, cyclic use of heat or ice may help better than one alone.
Does massage help sciatica?
Massage is one of the modalities of adjuvant therapy for sciatica can be helpful and can decrease pain by strengthening the muscles as well as stretching the nerves. Deep massage can also help decrease the muscle spasms that develop in patients with sciatica.
Where to put an ice pack for sciatica?
For sciatica, an ice pack or even a heating pad can be used by placing it into the lower back and the gluteal region. It helps decrease the inflammation of the nerve there and thereby decreasing the pain and associated symptoms.
Does the inversion table help sciatica?
Inversion table similar to traction helps sciatica by increasing the height of the disk and thereby allowing the disk to go back into space thereby decreasing the compression of the nerve root may help in decreasing the pain of sciatica. The issue of inversion table as well as traction is that this is effective until the patient uses them and once the patient is upright and moving, the effect of the inversion table or the traction may not be persistent.
Can the sciatica cause ankle pain?
Sciatica or lumbar radiculopathy causes pain radiating from the back or the hip into the lower extremities down the leg. The pain radiates along the back or the side of the thigh and leg and radiates down foot. An isolated ankle pain may not be caused by radiculopathy. If the pain is on outer or inner side of the ankle and is radiating down or coming from the top then it may be associated with sciatica or lumbar radiculopathy.
Does sciatica get worse before it gets better?
90% of patients with sciatica will eventually get better in a period of four to six weeks. During this time, the pain may worsen also or it may keep on improving. Patients who have severe pain with or without tingling or numbness usually will need medical attention to relieve their pain during this duration. The treatment may involve medications, physical therapy and cortisone shots. Patients who have sudden onset of neurological deficit or weakness or worsening of the neurological deficit may need surgery also.
Can stress cause sciatica?
Sciatica like any other neurologic pain can have relation with the mental status and cognitive functions of the person. Though stress may directly not be the causative factor for sciatica, it may have its effect on the severity as well as course of the disease process of sciatica. Patients with high stress levels may have difficulty coping with sciatica and may take longer time to get better.
What happens if sciatica left untreated?
Sciatica in most patients will get better by itself in a period of four to six weeks. The pain as well as tingling and numbness tend to improve over time, though it may have periods of worsening. Patients may need treatment in the form of medications or injections to relieve the pain, so as to spend this period of four to six weeks, till then the relief is evident.
Occasionally in about 10% of the patients, there will be no relief, worsening or recurrence of sciatica pain despite all treatment modalities over four to six weeks. These patients may need surgical management to relieve their pain due to the pressure over the nerve roots.
Can sciatica be a serious disorder?
Sciatica is usually self limiting in 90% of patients and only needs treatment in the form of medication and physical therapy and occasionally cortisone injection. In about 10% of patients, this may not be relieved by any modality and these patients may need to undergo surgical treatment.
Sciatica can also rarely lead to rapid neurological deficit presenting in the form of cauda equina syndrome, which can be potentially disabling. The neurological deficit caused due to cauda equina syndrome may be permanent especially if not treated early in the disease process. Such patients may not only have weakness in their legs, but may also lose control over their bowel and bladder, which may or may not recover over time.
What are the medication that can help sciatica?
Sciatica pain can be relieved by the help of anti-inflammatory medications like ibuprofen, naproxen. It can also be helped by Tylenol. Stronger pain medications like tramadol and narcotic medications may occasionally be needed for a short period of time.
Neuromodulator medications like gabapentin and pregabalin may also be helpful in decreasing the sciatica pain. Occasionally, medications like amitriptyline, duloxetine and carbamazepine may also be used in some patients to relieve their pain.
Is the back brace helpful for sciatica pain?
Back brace may be helpful in patients who have back pain with or without sciatica. Patients who have only radicular pain in their lower extremity may not be helped by the back brace. Use of back brace for a long period of time may be detrimental by causing atrophy of the back muscles.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://stage.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
